Non-pharmacological therapies for chronic stress
PDF
What is the best way to overcome stress? It is undoubtedly to learn to adapt to it! Stress, defined as a non-specific response of the body to any type of stimulus, is a normal phenomenon to which we are all exposed. Faced with any external aggression (from our environment) or internal aggression (from the body itself), stress is a physiological response of adaptation that allows us to maintain the body’s balance. At the psychological level, this response involves cognitive, emotional and behavioral processes. When stress is prolonged (chronic stress), it can have negative consequences on our organism both biologically and behaviorally. This article deals with the biological aspects underlying the deleterious – but also positive – effects of stress exposure. We will see what are the determinants underlying the effects of stress. We then propose a review of non-pharmacological techniques to help us manage the stressful experience, thus offering some tools to develop our adaptive skills.
1. Stress, a physiological adaptation response
In the face of any external (from the environment) or internal (from the organism itself) aggression, stress constitutes a physiological response of adaptation allowing the organism to maintain its homeostasis. At the psychological level, this response involves cognitive, emotional and behavioral processes. The return to homeostasis allows us to move towards a state of well-being as defined by the World Health Organization: “a state of complete physical, mental and social well-being, [which] is not merely the absence of disease or infirmity” [2].
When the effect of the stressor (also known as a stressor) is prolonged over time, there is a risk that maladaptation may occur, exposing the individual to a state of vulnerability or even a pathological state, characterized by a significant impact on his or her functioning. This state is characterized by a disruption of the biological, cognitive, emotional and behavioral balance. There is inter-individual variability in the vulnerability to develop a pathology during chronic exposure to a stressor (Figure 1). It should be noted here that chronic stress is not strictly speaking a disease, i.e. an “alteration of the physical or mental functions of a person causing suffering” [3], but rather a factor that triggers or aggravates a pre-existing condition or vulnerability to a medical pathology.
Stress – defined as the systemic response of the organism – may in some cases decompensate, i.e. reveal, pathological states of all systems (neuropsychiatric, cardiovascular, gastrointestinal, endocrine, immunoinflammatory, etc.). Moreover, although clinical research has developed ways of characterizing chronic stress (by the disruptions it induces at the hormonal, neuronal and cerebral levels; see below), there is currently no validated clinical diagnostic test that would allow a physician to objectify a patient’s chronic stress state. The measurement of the effects of interventions (pharmacological or not) aimed at reducing chronic stress is based on the subjective feeling of the subject. Although the biological response to stress can be measured, such as the concentration of cortisol in the blood, this marker is not used in current practice to diagnose a state of acute or chronic stress.
This article will discuss non-drug strategies to help manage chronic stress. First, we will discuss the biological effects of chronic stress and the challenges of controlling its consequences. Then we will present the physiological and psychological risks associated with chronic stress. Finally, we will develop the various non-pharmacological interventions aimed at preventing the deleterious effects of chronic stress.
2. Why manage the biological effects of chronic stress? The science behind it
Exposure to stress is an integral part of our daily lives. As defined in the introduction, stress can be more or less intense and prolonged. Depending on the intensity and duration of exposure to stressful phenomena, the effects on the body will be different, ranging from the development of adaptive skills to the appearance of a pathological state. The purpose of this section is to raise awareness of the different levels of stress, their biological effects, the concept of allostatic load, as well as the inter-individual variability in vulnerability to stress. The definition of these concepts will allow the identification of potential targets for non-pharmacological therapies for chronic stress and their expected effects on biology.
Classically, three levels of stress are distinguished according to their intensity and duration. It should be noted that the perceived intensity of stress depends on individual vulnerability to stressors. Indeed, this vulnerability is a function of a certain number of innate (genetic) and acquired factors (early exposure to stressors, social environment, exposure to toxic substances, epigenetics). A three-level classification of stress was proposed by Shonkoff and colleagues in 2009 [4]:
- Physiological stress, of short duration (minutes to hours) in response to stimuli perceived by the individual as mild to moderate.
- Tolerable stress, which can be chronic mild stress (a few days to a few months) or short-term intense stress. It exposes the individual to physiological responses that are potentially damaging, but which result in a return to a state of homeostasis. These responses can even help protect against future stressors by allowing the development of better adaptive capacities.
- Toxic stress, or chronic stress (a few months to a few years), exposes the individual to damaging physiological reactions occurring under conditions of severe adversity considered to be beyond the individual’s internal and/or external adaptive resources. Toxic stress exerts deleterious effects on the biological system of regulation and adaptation to the stressor, and consequently causes damage at several levels: molecular, neuronal and neurofunctional.
2.1. The hormonal consequences of stress
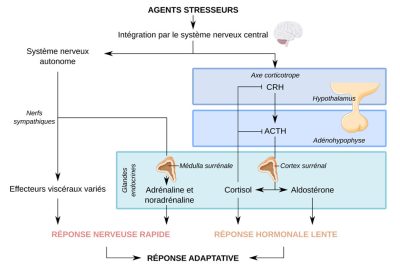
In addition to the corticotropic axis, several other physiological reactions have a significant influence on the effects of stress on the biology of the individual. Indeed, metabolic abnormalities (release of excitotoxicExcitotoxicity is a pathological process of neuronal damage and destruction or neurotoxicity, by hyperactivation by glutamic acid and its analogues (all being excitatory neurotransmitters). amino acids) as well as anti or pro-inflammatory mechanisms affect neurons in brain regions – such as the hippocampus, amygdala, and frontal cortex (Figure 3) – supporting key cognitive functions in adaptation to any stressor.
2.2. Effects of stress at the molecular and synaptic level
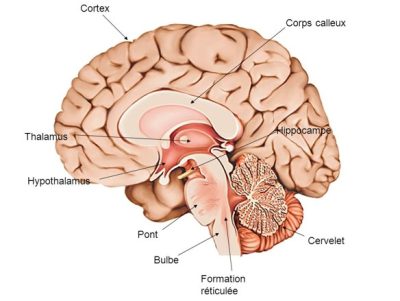
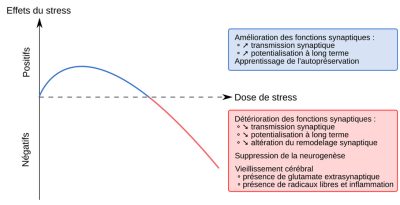
These changes in neurotransmission involve regions particularly vulnerable to excitotoxicity such as the hippocampus, prefrontal cortex, and amygdala. Glutamate and corticoid hormones play a central role in the effects of stress on the structure and function of neurons in these brain regions. Indeed, their secretion and cascading reactions will have consequences such as [8],[9]:
- The alteration of the synaptic function of the elicited brain regions, as these are involved in learning and behavior selection.
- Decreased synaptic plasticity: reduced dendritic remodelling and neurogenesis.
- Impairment of neuronal life: increased excitotoxicity – mainly due to excess glutamate released in the synaptic cleft – eventually leading to possible neuronal death. Note that this neuronal death leads to a local inflammatory response and to the production of deleterious free radicals.
Depending on the duration of exposure and the intensity of the stressor, these effects are either protective and stimulate brain plasticity (physiological and tolerable stress) or deleterious and damaging to the brain (toxic/chronic stress) (Figure 4).
2.3 Effects of stress on brain structure and function
First of all, the hippocampus is a region rich in mineral and glucocorticoid receptors and, consequently, is sensitive to the presence of too many of these molecules in case of chronic exposure to the stressor. This can lead to the loss of dendritic spines, structures that play a key role in synaptic function and neuronal plasticity. Also, these physiological alterations have repercussions on the functions of the hippocampus such as spatial and episodic memory as well as mood regulation. These impairments have consequences on cognitive functions, which are essential for the implementation of emotional and behavioral strategies for coping with stress.
Moreover, the cerebral amygdala, well known for its role in the processing of emotional information, is largely involved in stress and mood regulation. In contrast to what happens in the hippocampus, acute and chronic stress lead to an increase in the density and number of dendritic spines in a region of the amygdala called the basolateral nucleus. In addition, chronic stress results in a reduction of dendrites in the medial nucleus. These histological changes have been described as being involved in the increase in anxiety and behaviors related to post-traumatic stress.
Finally, the loss of connections and pruning of dendrites in the medial prefrontal cortex have been linked to cognitive rigidity – defined as the inability to change one’s thought patterns despite negative consequences – which potentially impacts the individual’s ability to develop adaptive strategies in response to the stressor. Increased neural dendrites in the orbitofrontal cortex have been linked to hypervigilance. The prefrontal cortex as a whole is also vulnerable to stress by showing deficiencies such as loss of adaptive capacities and memory disorders (accelerated aging).
In summary, stress acts on the structure and functioning of key brain regions in cognitive functions, emotion regulation and behavioral aspects, which are themselves crucial in the development of adaptive strategies to stressors. Thus, damage to these structures leads to a vicious circle at the end of which the ability to adapt to the stressor is impaired. In addition to innate and/or acquired vulnerability, the neurotoxic effects of glucocorticoid secretion accentuate the pre-existing state of biological vulnerability, thus creating a vicious circle of chronic stress.
2.4. Inter-individual variability of vulnerability to stress
Faced with various stressors, there is individual variability in the ability to adapt [5,9,10]. This individual vulnerability is conditioned by genetic inheritance, stressful experiences during development and their consequences on the genetic expression of proteins involved in stress regulation mechanisms. Thus, the earlier an individual is exposed to stressors during his or her life, the more adverse consequences he or she will experience on his or her brain development, in particular concerning the specialization of neuronal cells in key adaptation regions. There is thus an interrelation between the genetic heritage and the environment of the individual throughout life. This theory of gene-environment interaction explains individual trajectories ranging from strong adaptive capacities to stressors to the development of stress-related psychiatric pathologies such as depression or anxiety disorders, among others.
3. The concept of allostasis and allostatic load
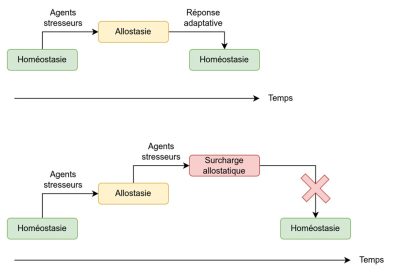
Later, Mc Ewen [9] completed the theory of allostasis suggesting that “stress hormones that are essential to the survival of the species may have adverse effects on physical and mental health if secreted over longer periods of time“. Thus, the concept of allostatic load corresponds to the accumulation of stresses applied to the biological system – primarily the corticotropic axis – over time. Thus, it can be conceptualized as the price to pay for prolonged adaptation to the stressor. Taken together, the concepts of allostasis and allostatic load make it possible to account for the dynamics of response to stress. Indeed, the perceived stress will depend on the individual’s past experience, genetic heritage, and the behavioral strategies put in place. When the brain identifies an experience (internal or external) as stressful, physiological and behavioral responses will be initiated, defining the allostasis mechanism. Over time, in the event of repeated or intense exposure to the stressor, allostasis – enabled by the neuronal, endocrine (corticoid hormones), and immuno-inflammatory response – will be over-solicited and thus accumulate allostatic load. Thus, the more the allostatic load is increased, the greater the risk of deleterious consequences on the organs. Chronic exposure to the stressor will therefore lead to an increased risk of deregulation of the body’s homeostasis, as a result of a cascade of inflammatory, immunological and metabolic processes. The long-term consequences are the risk of developing cardiac, immune, metabolic and neuropsychiatric pathologies. These concepts are summarized in Figure 5.
4. What are the available interventions based on the scientific data on the biological effects of stress?
In summary, all the scientific data on the physiological response to stress make it possible to identify lines of action and/or prevention in order to prevent any long-term consequences of chronic exposure to a stressor. The strategies will be either preventive, aimed at reinforcing adaptive strategies, or therapeutic in case of development of a psychiatric pathology such as mood disorder or anxiety disorder. Here, we will not deal with therapies specific to psychiatric pathologies, although some of them are common to the therapy focused on stress management.
The common objective of all non-pharmacological techniques is to promote coping capacities to stress on the emotional, cognitive and behavioral dimensions, but also on the scale of brain biology. The aim is to reduce the allostatic load linked to the accumulation of the deleterious effects of the stressor over time. We can schematically identify several potential levels of action:
- Emotional: emotion regulation techniques;
- Cognitive-behavioral: identifying and distancing oneself from potentially stressful environmental factors, learning positive coping strategies, reinforcing virtuous behaviors;
- Biological: hygienic and dietary rules concerning diet, sleep, sports activity, reinforcement of positive social support.
4.1. Action on the environment
In order to prevent chronic exposure to stressors, action on the environment is crucial. Ergonomics in the workplace, discussion groups, specific actions for the different professions, work rhythms, numerous prevention axes exist.
4.2. Early intervention

Stress in the pregnant mother has effects on both the obstetrical prognosis (premature delivery, intrauterine growth retardation, risk of pre-eclampsia, gestational diabetes) and the developmental prognosis of the child (attachment disorders, asthma, allergies, mood disorders) [12]. Prevention strategies as well as cognitive-behavioral psychotherapies allow us to accompany the mother-to-be and her partner in this important life event that is parenthood. Mindfulness-based techniques, cognitive-behavioral therapies, relaxation techniques and yoga have all been shown to be effective in managing stress and anxiety in pregnant women. In the postpartum period, the 1000 days program [13] developed by a commission of experts in 2020 proposes a certain number of preventive actions underlining the importance of this crucial period for the development of the newborn. This report [12] describes it as “a sensitive period for the development and security of the child, which contains the premises for the health and well-being of the individual throughout life.”
Therefore, the identification of potential stressors, neglect and even abuse at the family level are at the heart of public health policies. In France, the Maternal and Child Protection (PMI) services have, at the departmental level, missions of health protection for mothers and children. They carry out medical and social prevention and monitoring of pregnant women, parents and children under 6 years of age (Figure 6).
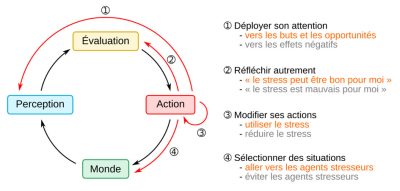
Finally, the school is a good place to implement prevention activities. Many programs have been developed, based on the appraisal model proposed by Lazarus and Folkman in 1984 [14]. These approaches have been the object of the development of numerous teaching programs in order to provide children with psychotherapeutic tools, of cognitive and behavioral inspiration, and thus optimize their adaptive capacities.
4.3. Cognitive-behavioural approaches
Cognitive-behavioural therapy is a form of psychotherapy based on a functional analysis of the subject’s behaviour. The objective is first to identify inappropriate behaviours in a given context (e.g., a phobia of flying). Then, the subject and the therapist will work on defusing the learned “inappropriate” behavior in the face of the situation. Finally, the work will focus on learning a behavior that has fewer negative consequences and in particular less suffering for the individual. This technique has been the subject of numerous clinical studies which have demonstrated its effectiveness, particularly in the area of stress regulation [15]. On the neurobiological level, cognitive and behavioral techniques have shown effects on the volume of the prefrontal cortex (in the case of the treatment of chronic fatigue) as well as the amygdala (in the treatment of chronic anxiety).
Since the 1980s, many therapies based on this cognitive and behavioral approach have been developed. They have been adapted to emotional regulation and the development of stress reduction strategies. Cognitive and behavioral therapies are practiced by psychotherapists who are certified and trained specifically in this technique. The French Association of Cognitive and Behavioral Psychotherapy [16] is the main training structure in France. Their website provides a directory of accredited psychotherapists.
4.4 Interventions focused on emotion regulation techniques
The importance of emotion regulation in order to maintain a form of psychic homeostasis and to decrease the allostatic load was underlined by the theory of Campos and colleagues in 2004 [17]. Indeed, these authors point out that emotions are fundamental in the processes of decision making and adaptation of behaviors by their influence on cognitive processes. They therefore play a protective role. On the other hand, when these emotions are not regulated, they can have harmful effects on the psychological and physiological dimensions of the individual.
4.4.1 Relaxation and breathing techniques
Breathing and relaxation techniques are ancestral stress management techniques. Their mechanism of action is based on the control of physiological responses to stress such as the increase in breathing frequency, muscular tension, and the emergence of anxiety-provoking mental images. The techniques of deep breathing, control of breathing frequency and guided mental imagery have demonstrated their effectiveness (Figure 7). They also have the advantage of being accessible, with the possibility of carrying out exercises anywhere, at any time, and by the subject himself [18].
4.4.2. Mindfulness therapy
Mindfulness-based stress reduction [19] is an intervention that has been shown to be effective in reducing stress, depression and anxiety [20] (Figure 7). It can also be used in so-called “non-clinical” populations, i.e., those without psychiatric pathology. The principle of mindfulness is based on different exercises such as body scanning, meditation and yoga. Mindfulness aims to change the individual’s relationship with certain thoughts or stressful events by reducing emotional reactivity and promoting cognitive reappraisal. A standard course of treatment is an 8-week group course with 2.5 hours per week of group sessions and a 6-hour retreat [20]. Several variants of mindfulness meditation have been developed, such as digital forms, which have allowed a wide diffusion of this practice. Many studies have been conducted on the use of mindfulness in “non-clinical” populations. A meta-analysis has documented the effects of this technique on 2668 people. Thus, it was reported that there was a decrease in anxiety and depressive symptoms, associated with an improvement in quality of life [20].
4.4.3. Integrative stress optimization model – when the stressor can be used as an asset
4.4.4. Physical activity
Regular physical activity is an effective therapy that acts biologically on several levels of the stress regulation system. Indeed, it increases cerebral blood flow in the prefrontal and parietal cortex and improves executive functions. The latter correspond to a set of higher cognitive functions such as planning, organization and strategy development. They are essential for the implementation of adaptive strategies in the face of any form of stressor. In addition, regular physical activity has been shown to increase the volume of the hippocampus, which is involved in stress regulation and maladaptation mechanisms. Finally, regular physical activity is now well known for its antidepressant and protective effects against cardiovascular disease and dementia as well as prevention of premature aging [22].
In total, sport will act on the structure and function of brain regions playing a preponderant role in the regulation of stress and its consequences (psychological, cardiovascular, metabolic and cognitive).
4.4.5. Positive social support
Social integration, social support, and the search for meaning are all approaches that can reduce the allostatic load. Programs such as “Experience Corps”, aimed at elderly subjects and based on the development of cognitive functions associated with coping strategies in addition to physical activity, have proven to be effective in decreasing cognitive decline and improving mental health, with effects on cerebral blood flow in the prefrontal cortex [23]. Other programs such as the “DeStress for Success Program” [24] have been developed for young populations and focus on identifying the stressor and working on coping strategies (Figure 8 illustrates the choice of the mammoth as the logo for the “DeStress for Success” program). They have an effect on the hormonal responses to stress, such as the reduction of cortisol hypersecretion [6]. This work sheds light on the effects of non-pharmacological therapies on the biological system of the stress response.
5. Messages to remember
- Stress, defined as a non-specific response of the organism to any type of solicitation, is a normal phenomenon to which we are all exposed.
- If it is prolonged and/or intense, the cascading biological and behavioral reactions may lead to a form of maladaptation of the individual with biological and behavioral consequences.
- Non-pharmacological stress management techniques are characterized by the reinforcement of adaptive capacities on the emotional, cognitive and behavioral dimensions, with repercussions on the scale of the brain biology.
- These therapies aim to decrease the allostatic load related to the accumulation of the deleterious effects of stress over time.
- Individual vulnerability to stress is a function of a number of innate (genetic) and acquired (social environment, epigenetics) factors.
- The ultimate goal is to limit the impact of the imbalance caused by the stressor, or even to use this imbalance to develop individual resources focused on the homeostatic maintenance of the biological systems underlying cognitive, emotional and behavioral processes.
This article was originally published in December 2022 by Planet Vie under a Creative Commons license : Non-drug therapies for chronic stress. It was edited by M Pascal Combemorel, Editorial Manager of Planet-Vie.
Notes and References
Cover image. [Source: CIPHR Connect, CC BY 2.0 <https://creativecommons.org/licenses/by/2.0>, via Wikimedia Commons]
[1] Fink, G. (2017) Stress: Concepts, Definition and History. In Reference Module In neuroscience and Biobehavioral Psychology, Elsevier Inc, Amsterdam, 1-9.
[2] Preamble to the Constitution of the World Health Organization, as adopted by the International Conference on Health, New York, June 19-22, 1946
[3] Academy of Medicine, 2022, “Disease – Dictionary of the National Academy of Medicine”
[4] National Scientific Council on the Developing Child.(2005/2014). Excessive Stress Disrupts the Architecture of the Developing Brain: Working Paper 3. Updated Edition.
[5] Lupien SJ, McEwen BS, Gunnar MR & Heim C., 2009, “Effects of stress throughout the lifespan on the brain, behavior and cognition”, Nat. Rev. Neurosci.;10(6):434-45. doi: 10.1038/nrn2639. Epub 2009 Apr 29.
[6] Lupien SJ, Juster RP, Raymond C, Marin MF., 2018, “The effects of chronic stress on the human brain: from neurotoxicity, to vulnerability, to opportunity”, Front Neuroendocrinol. 49:91-105. doi: 10.1016/j.yfrne.2018.02.001. Epub 2018 Feb 5.
[7] such as glutamate, GABA, acetylcholine, norepinephrine and serotonin.
[8] McEwen BS, Bowles NP, Gray JD, Hill MN, Hunter RG, Karatsoreos IN, & Nasca C., 2015, Mechanisms of stress in the brain. Nat Neurosci. 18(10):1353-63. doi: 10.1038/nn.4086. Epub 2015 Sep 25. PMID: 26404710; PMCID: PMC4933289.
[9] McEwen BS., 1998, Protective and damaging effects of stress mediators. N Engl J Med. 338(3):171-9. doi: 10.1056/NEJM199801153380307. PMID: 9428819.
[10] McEwen BS, Eiland L, Hunter RG, & Miller MM., 2012, Stress and anxiety: structural plasticity and epigenetic regulation as a consequence of stress. Neuropharmacology. 62(1):3-12. doi: 10.1016/j.neuropharm.2011.07.014. Epub 2011 Jul 27. PMID: 21807003; PMCID: PMC3196296.
[11] Sterling P. & Eyer J, 1988, Allostasis: a new paradigm to explain arousal pathology, Handbook of Life Stress, Cognition and Health. J. Wiley Ltd. Edited by Fisher S., Reason J. (eds), 629-649.
[12] Coussons-Read, M.E., 2013, Effects of prenatal stress on pregnancy and human development: mechanisms and pathways. Obstet Med. 6(2):52-57. doi: 10.1177/1753495X12473751. Epub 2013 May 3. PMID: 27757157; PMCID: PMC5052760.
[13] Report of the first 1000 days commission (Ministère Des Solidarités Et De La Santé), September 2020.
[14] Lazarus R. S. & Folkman S. (1984). Stress, Appraisal, and Coping. New York. New York, NY: Springer.
[15] van Dis EAM, van Veen SC, Hagenaars MA, et al. Long-term Outcomes of Cognitive Behavioral Therapy for Anxiety-Related Disorders: A Systematic Review and Meta-analysis. JAMA Psychiatry. 2020;77(3):265–273. doi:10.1001/jamapsychiatry.2019.3986
[17] Campos JJ, Frankel CB & Camras L., 2004, On the nature of emotion regulation. Child Dev. 75(2):377-94. doi: 10.1111/j.1467-8624.2004.00681.x. PMID: 15056194.
[18] Magnon V., Dutheil F. & Vallet G.T., 2021, Benefits from one session of deep and slow breathing on vagal tone and anxiety in young and older adults. Sci Rep. 11(1):19267. doi: 10.1038/s41598-021-98736-9. PMID: 34588511; PMCID: PMC8481564.
[19] In its 2021 report, the Interministerial Mission of Vigilance and Combat against Sectarian Aberrations (Miviludes) emphasizes that the absence of a precise and univocal definition of mindfulness meditation may present a “risk of deviation of the practice to the benefit of sectarian aberrations. It also notes that, more generally, “most new personal development techniques are based on uncontrolled training and qualifications”. People wishing to use mindfulness meditation should therefore ensure that they are supervised by professionals who have undergone training and who use the practices defined by cognitive and behavioral therapy societies, such as the AFTCC.
[20] Khoury B., Sharma M., Rush S.E. & Fournier C., 2015, Mindfulness-based stress reduction for healthy individuals: A meta-analysis. J Psychosom Res. 78(6):519-28. doi: 10.1016/j.jpsychores.2015.03.009. Epub 2015 Mar 20. PMID: 25818837.
[21] Crum A.J., Jamieson J.P. & Akinola M., 2020, Optimizing stress: An integrated intervention for regulating stress responses. Emotion. 20(1):120-125. doi: 10.1037/emo0000670. PMID: 31961190; PMCID: PMC7608610.
[22] Arida R.M. & Teixeira-Machado L., 2021, The Contribution of Physical Exercise to Brain Resilience. Front Behav Neurosci. 14:626769. doi: 10.3389/fnbeh.2020.626769. PMID: 33584215; PMCID: PMC7874196.
[23] Carlson M.C., Erickson K.I., Kramer A.F., Voss M.W., Bolea N., Mielke M., McGill S., Rebok G.W., Seeman T. & Fried L.P., 2009, Evidence for neurocognitive plasticity in at-risk older adults: the experience corps program. J Gerontol A Biol Sci Med Sci. 64(12):1275-82. doi: 10.1093/gerona/glp117. Epub 2009 Aug 19. PMID: 19692672; PMCID: PMC2781785.
[24] https://www.stresshumain.ca/programmes/de-stresse-et-progresse/
The Encyclopedia of the Environment by the Association des Encyclopédies de l'Environnement et de l'Énergie (www.a3e.fr), contractually linked to the University of Grenoble Alpes and Grenoble INP, and sponsored by the French Academy of Sciences.
To cite this article: BATAIL Jean-Marie (June 26, 2023), Non-pharmacological therapies for chronic stress, Encyclopedia of the Environment, Accessed December 22, 2024 [online ISSN 2555-0950] url : https://www.encyclopedie-environnement.org/en/health/non-pharmacological-therapies-for-chronic-stress/.
The articles in the Encyclopedia of the Environment are made available under the terms of the Creative Commons BY-NC-SA license, which authorizes reproduction subject to: citing the source, not making commercial use of them, sharing identical initial conditions, reproducing at each reuse or distribution the mention of this Creative Commons BY-NC-SA license.