From smallpox to Mpox: a renewed threat
PDFSmallpox: a brief history of a controlled plague. Of all the plagues that have afflicted humanity, human smallpox is undoubtedly one of the most terrifying. A highly contagious viral disease, humanity has been subjected to this scourge for centuries, and in particular for the last 3,000 to 4,000 years. The disease, transmitted by close contact, was encouraged by increasing human density, growing urbanisation, wars, colonisation and population movements. Decimating populations for millennia, leaving indelible skin scars on survivors, it was customary not to count one’s children until after they had contracted the disease: smallpox could affect over 90% of the population, and a third of those infected died, particularly children (case-fatality rate 30%)[1].

Biological risk. Even when it has been eradicated, smallpox is still a potential danger, and one of the threats posed by bioterrorism. This is why many doses of smallpox vaccine are still kept, particularly by the military, and why research into vaccines against the various forms of smallpox has never been halted. There are currently three highly effective smallpox vaccines (MVA-BN, LC16, OrthopoxVac). These vaccines are also effective against other animal poxviruses.
Animal poxviruses. Unlike ‘smallpox’, which only affected humans, other viruses of the same genus (Orthopoxviruses) are present and widespread in the animal world, such as bovine pox, camel pox, avian pox and monkey pox. These viruses, all of which share a common ancestor with the human smallpox virus, can also occasionally infect humans, but without causing serious illness or sustained human-to-human transmission.
The Mpox virus or monkeypox virus belongs to the same genus of Orthopoxviruses as the human smallpox virus. It was first isolated in 1958 from a group of monkeys imported to Copenhagen, Denmark, hence its name. There are currently two main types of Mpox virus: clade 1, found in the Congo River basin in Central Africa, and clade 2, found in West Africa. It circulates locally in its natural state in certain African countries, where it mainly infects rodents (rats, squirrels, etc.), and is occasionally transmitted to other species. As a result, sporadic Mpox infections have been observed in humans for several decades, mainly in Africa, but without causing epidemics or, a fortiori, pandemics, according to the classic pattern of a zoonosis with no effective direct human-to-human transmission. In 2022, this classic pattern changes, with the emergence of a variant (Clade 2b) that is more easily transmitted between humans, that leaves the African continent and causes epidemic outbreaks with a low but significant lethality (of the order of 0.2% in Europe): we are faced with the emergence of a zoonosis with direct human-to-human transmission, potentially fearsome, and which could in time give rise to fears of a resurgence of smallpox.
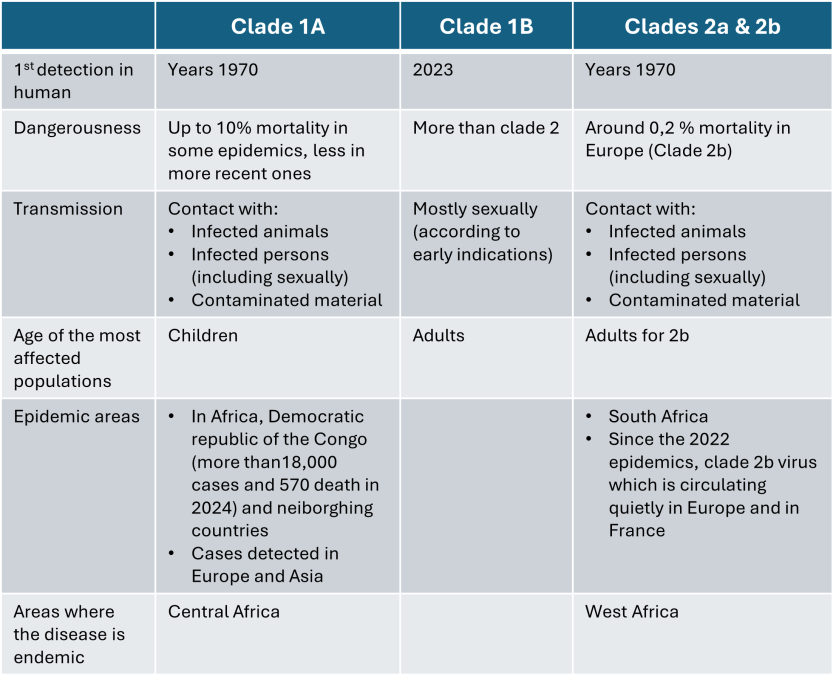
Table. The different types of Mpox (based on data from the literature). Clades refer to variations of the same virus that have diverged through genetic mutations.
Mpox (or monkeypox), the disease. Since the discovery of this viral disease in humans in 1970 in the Democratic Republic of Congo (DRC), small localised epidemic outbreaks have been observed in certain Central and West African countries: DRC, Congo, Liberia, Sierra Leone, Nigeria, Côte d’Ivoire, South Sudan, etc. The disease remains rare and does not spread to the human population, but the frequency of epidemic outbreaks is increasing regularly. Between 2017 and 2019, more than 3,000 cases were recorded in Nigeria, the DRC and the Central African Republic.

Mpox’s first escapades outside Africa. Until 2022, the disease was only detected very sporadically outside Africa, and always during infections imported from Africa, without being followed by human-to-human transmission. In 2003, the virus first spread to the United States from Ghana via rodents imported from a pet shop. 47 cases were biologically confirmed, but no human-to-human transmission or deaths were reported. From 2018, a few imported cases linked to travellers from Nigeria appeared in the United Kingdom, Israel, the United States and Singapore, signalling ongoing transmission in West Africa and early signs of international spread.
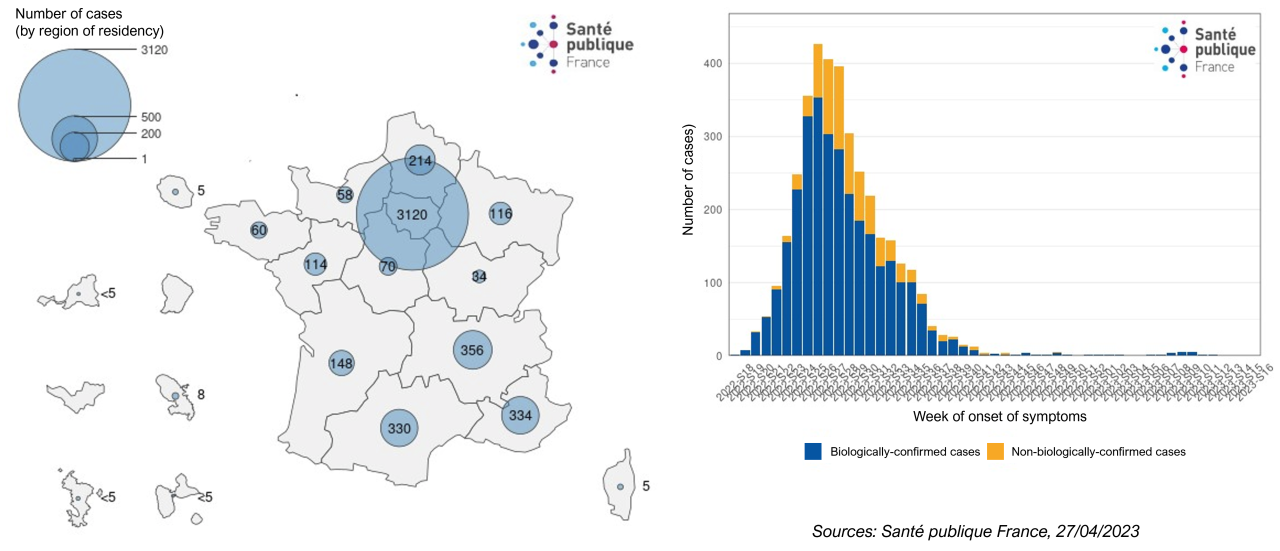
2022, the start of an unexpected pandemic. In May 2022, cases of monkeypox increased dramatically in previously unaffected regions, with unprecedented human-to-human transmission. In response, the WHO declared a public health emergency of international concern in July, and global health measures were launched, including surveillance campaigns and vaccination of at-risk populations. The emergency was lifted in May 2023 after a sustained global decline in cases. In August 2024, there were almost 100,000 confirmed cases in 113 countries, and more than 200 deaths (case-fatality rate of 0.2%). The virus responsible for global transmission (clade 2b) has been transmitted between humans through close contact, particularly among men who have sex with men (MSM). Outside Africa, more than 99% of cases have occurred in men. The virus (clade 2b) is still circulating at a low level (between 12 and 26 cases per month in France between January and June 2024, Figure 3).
Facing up to the threat. Smallpox vaccines (MVA-BN, LC16, OrthopoxVac), whether attenuated or inactivated, provide effective protection (up to 85%) against other poxviruses, including the different clades of the Mpox virus. Vaccination against smallpox was discontinued in 1980 when smallpox was declared eradicated: people under 45 therefore have no immune protection against Mpox. People over the age of 45, who have in principle been vaccinated against smallpox, should a priori benefit from immune protection against Mpox, but the scientific data is still uncertain as to the long-term persistence of the immunity induced against Mpox by the smallpox vaccine.
As it is impossible to act on the factors that cause the disease to emerge (wild rodents) and difficult to act on the factors that cause it to spread (contacts and risky behaviour), vaccination of vulnerable populations is the preferred weapon for containing the current Mpox epidemic. Given the mode of transmission and epidemiology of the disease (which mainly affects MSM), widespread vaccination of the population is not currently envisaged.
Preparedness and the fight against the epidemic are focusing on the most vulnerable populations: endemic areas in Africa and MSM communities, particularly outside Africa. The strategy for combating the threat is to act on the vulnerability of exposed populations (vaccination, controlling behaviour and hygiene), and to monitor the presence of the threat to reduce transmission (case detection, contact tracing, rapid diagnostics).
Vaccine stocks are being built up everywhere to prepare for the possibility of mass vaccination should human-to-human transmission become widespread.
An uncertain future. Faced with the emergence of a contagious zoonosis caused by close proximity or simple contact between humans, the utmost vigilance is called for, and the WHO was quick to issue a worldwide alert [3, 4]. But unlike other emerging pathogens (Ebolavirus, coronavirus, influenza, etc.), humanity already has effective vaccines against Mpox. If these vaccines are produced and distributed in good conditions, if hygiene and behavioural measures are respected, if surveillance and rapid detection of cases are effective and transparent, the Mpox epidemic should be brought under control and the disease rapidly contained, as was the case in 2022. But this virus has shown us twice in its recent history: natural wild strains persist in the heart of the tropical forest, evolve, infect a variety of hosts, are transmitted to humans, can adapt and, by chance or necessity, increase their pathogenic power. The shadow of smallpox persists…
Notes and references
Vignette. Mpox Virus (Poxviridae). Colorized transmission electron micrograph of mpox virus particles (red) found within an infected cell (blue), cultured in the laboratory. Image captured and color-enhanced at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland, USA. [Source: NIAID, CC BY 2.0, via Wikimedia Commons]
[1] Thèves C. Crubézy E. Biagini P. 2016. History of Smallpox and Its Spread in Human Populations. Microbiol Spectr 4:10.1128/microbiolspec.poh-0004-2014. https://doi.org/10.1128/microbiolspec.poh-0004-2014
[2] Sourav Saha, Trina Chakraborty, Rejwan Bin Sulaiman, Tithi Paul A Comparative Analysis of CNN-Based Pretrained Models for the Detection and Prediction of Monkeypox
[3] https://www.lemonde.fr/planete/article/2024/08/15/pourquoi-l-oms-a-classe-l-epidemie-de-mpox-en-afrique-urgence-de-sante-publique-de-portee-internationale_6281426_3244.html (in french)
[4] https://www.lemonde.fr/les-decodeurs/article/2024/08/21/mpox-clade-zoonose-le-lexique-pour-comprendre-les-mots-qui-circulent-avec-ce-virus_6289426_4355770.html (in french)