Exposome and social sciences: the promise of a meeting?
PDF
The concept of exposure aims to identify the complex causes of chronic diseases related to the environment. It builds on knowledge that has been well established in epidemiology for at least forty years, potentially creating a bridge between disciplines interested in environmental health (medicine, biomedical sciences, epidemiology, social sciences). This text proposes to see how, under the banner of the exposome, we can envisage intensified collaborations between all these disciplines that question socio-environmental determinants, and how the implementation of these collaborative works can still prove difficult today. The contribution of the social sciences to environment-related health issues still faces the relative closure of the approach and methods developed by the biomedical sciences, and by epidemiology in particular. Conversely, social scientists themselves may be reluctant to work in tandem with sciences that do not study social relations as such, and systematically quantify and individualize the phenomena they observe. The potential for interdisciplinary collaboration in exposures requires the design of research programmes covering a broad spectrum of approaches and methods, from the measurement of biomarkers by molecular biology to an ethnographic study of living and working conditions.
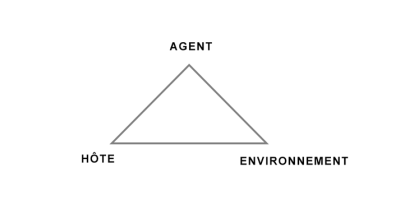
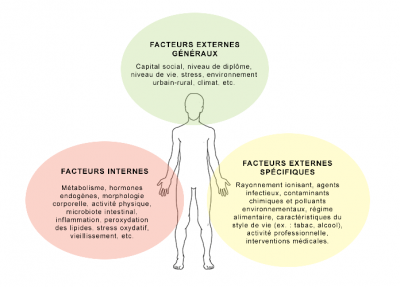
The third National Health and Environment Plan (PNSE3, 2015-2019) highlighted the concept of exposure as a key to understanding the complexity of exposures to pathogens responsible for many chronic diseases. Article 1 of Act No. 2016-41 [1] on the modernization of our health system, passed in 2016, consolidated this first institutional step, by stipulating that monitoring the state of health of the population and its determinants must be based on the exposome, understood as “the lifelong integration of all exposures that may influence human health”.
Borrowed from epidemiology, the notion of exposome was first proposed in 2005 by Christopher P. Wild [2] who has been involved for a long time in research on the environmental aspects of carcinogenesis. The notion of exposome – which presents a hermetic technical approach – is therefore included in a major law reforming the health system of President Holland.
This article proposes: a) to explain the notion of exposome from a historical perspective; b) to place the exposome within a broad disciplinary framework that includes epidemiology [3], biomedical sciences and social sciences. How can we define “environment” and “health” (in particular its social determinants) to ensure that all the disciplines concerned work together?
1. Exposure, mirror and complement of the genome
1.1. A brief history of the exposome
On October 12, 2018, PubMed – the most widely used search engine in the world in the fields of biology, medicine and epidemiology – lists 351 works whose title or abstract contains the word “exposome”, since the August 2005 original article. This number of studies is obviously modest compared to very broad and much older fields of biomedical knowledge (200,686 occurrences for “tuberculosis” at the same date, the first dating back to 1853). However, the growth in the volume of publications (there were only 260 one year earlier, for example) attests to a certain dynamic of research on the exposome, and the fact that health policy (PNSE3 and law n° 2016-41) has also brought itself into line with the exposome shows the interest generated by the notion. A closer examination of the publications reviewed by PubMed makes it possible to clarify matters: not only do doctors, toxicologists, epidemiologists and biologists use the exposome as a framework for their research on the toxicity of “exposures” to the human body, but they also regularly discuss the very notion of exposome in an attempt to determine its practical applicability.
In practice, the exposome is used to think about health in relation to the environment, and reflections are well underway on how to give it operational content. How to move from the concept of exposure to the practical implementation of research devices to measure it? What must be measured to discover harmful “exposures” to health, and how?
… But before we continue, let’s start by asking ourselves what the exposome is.
1.2. The public policy perspective
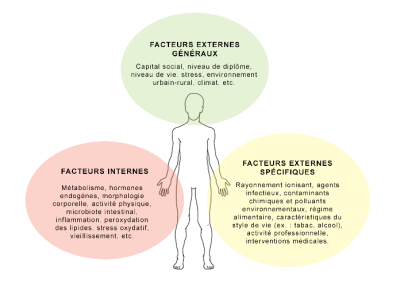
Several definitions of exposome were formulated during the vote on the January 2016 law. The one retained by Article 1 of the Act emphasizes that potentially harmful exposures to health can accumulate over a lifetime (Figure 1).
In the rest of the text, there is an explicit reference to exposures to ultraviolet rays, asbestos and ionizing radiation, as well as the definition of toxicovigilance as having as its purpose the “monitoring and assessment of toxic effects on humans” of exposure to substances which, whether natural or manufactured, may cause acute or chronic health problems. In all parliamentary debates, public actors are keen to find policies adapted to addressing the links between social phenomena and their health challenges.
The dissemination of the concept of the exposome in the public debate, in particular by Gérard Bapt, MP who initiated the registration of the exposome in the law, takes up the idea suggested by the title of Christopher P. Wild’s first article: the exposome is justified as an instrument for complementary knowledge of genetics to understand the incidence and development of chronic diseases. Not that medicine had ever imagined that chronic diseases could be explained by purely genetic factors. But the giant strides made by genome research in recent years have provided explanations for many diseases, and above all have made it possible to provide operational therapeutic approaches (particularly for cancers). The exposome aims to complement this approach and the privileged capacity of genetics to reason at the population level by exploring non-genetic determinants of health.
1.3. The Biomedical Sciences Perspective
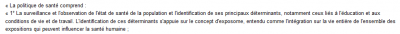
While the common representation of “environment” or “exposures” most often refers to toxic agents (such as asbestos, etc.), exposure is not reduced to them. In addition to these specific “external” agents (potentially toxic physical or chemical agents), it also includes socio-cultural, socio-economic and socio-environmental (“external general”) factors of our health (level of education, standard of living, urban living environment, etc.). The environment of organs also includes an internal dimension, made up of both physico-chemical elements such as hormones, mechanisms that regulate their secretion or regulation in the body (metabolism, oxidative stress, etc.) and elements that can be found in the human body, such as in the case of micro-organisms (fungi, viruses, bacteria, etc.) grouped under the term “microbiota” (read Human microbiotes: allies for our health).
In passing, we see how the exposome lends itself to multidisciplinarity, by inviting us to explore the social determinants of health and their interactions with biological processes.
The essential thing is to develop systemic research – exposure – on all parameters, from a globalizing, transversal point of view: the focus must be on health determinants, all now defined as environmental, and interacting with each other. Here again, it is understood that the exposome may have a great interest in soliciting a social science survey approach because, from this perspective, the diseases that a person living on the street may declare can no longer be understood as those suffered by a person with a high standard of living and who is in protected material (work, housing) conditions (see Environmental Inequalities).
In a very contemporary way, the exposome fits into the rapidly expanding landscape of “-omics” sciences and technologies, including “genomics”, which proposes to discover the “genome”. In this research on the biological determinants of health, however, it should be noted that exposure holds a special place: by “complementing” genomics, it embraces all other “internal” -omics approaches (Figure 2). Among these sciences, exposomics is therefore an interlocutor of genomics, which offers to synthesize the knowledge of other more analytical approaches -omics (metabolome, proteome, etc.). Proteomics thus aims to characterize all the proteins in the body, and metabolomics all the small molecules involved in metabolism.
Let’s go back to the question: how to make the measurement of the exposure operational? Its challenge is to respond to the gigantic enterprise of the GWAS (whole genome association study). Studying very many genetic variations in very many individuals, GWAS looks for possible links between genetic variations and variations in the characteristics of individuals (phenotypes). GWAS and exposomics come together with the intention of understanding why one person rather than another is likely to develop a chronic disease during their lifetime, taking into account the multiplicity of possible genetic combinations, in a multiplicity of possible environments.
Statistics and megadata (big data [4]) therefore play a crucial role in the possible dialogue between genomics and exposure. Tracing an individual’s exposure is a way of characterizing, through molecular biology, the specific signature (biomarkers) left by the effects of his exposures. But it is not enough to determine the relevant biomarkers to determine whether or not a person has been exposed to a toxic agent; exposures must also be investigated through questionnaires. The objective is to determine individual genetic susceptibilities, and to find correlations and modulations between diseases (identified by the alteration of a biomarker) and environmental factors (the three spheres presented in Figure 2). It is this approach that, overall, is behind the Human Early Life Exposome (HELIX) project, which tracks, for several cohorts recruited from different countries, a broad set of exposures in utero and during childhood, and examines their correlations with health states observed during childhood and with “molecular omics signatures” [5].
2. Studying environmental health through exposure: a difficult inter- or trans-disciplinarity
The exposomic approach does not invent the idea of collaboration between social sciences and biomedical sciences, but it offers in principle the opportunity to make this tandem more effective, through a systemic vision of the environment. In the study of internal cellular mechanisms, sociological and ethnographic work is combined to understand the material conditions and social practices that contribute to the socio-environmental determinants of health. This is what the proposal of the exposome potentially opens up. The intersection between all these disciplines is not new, if we remember the social concerns (hygiene and prevention, from a public health perspective) of epidemiology at its origins [6]. The dialogue between sociology and (social) epidemiology is old… and yet the “conflicts” [7] that have crossed epidemiology over the past three decades make interdisciplinary collaboration a hot topic. Over this period, epidemiologists have indeed opposed each other along at least two main lines of controversy: should epidemiology deal with social issues and what type of causality and interactions should it account for? The two questions are linked since entering into the depths of social contexts is a move away from reasoning that reduces risk factors to individual characteristics that, such as gender, tend to biologize the determinants of health [8].
In these fierce controversies, Ezra and Mervyn W. Susser, along with a few other South African public health physicians and epidemiologists, have been mediators, advocates of social epidemiology or “eco-epidemiology” that does not exclude other levels of analysis [9]. For them, studying the social conditions of existence and doing research in molecular biology are not mutually exclusive, quite the contrary.
However respected Susser’s reflection may be, however, the research avenues – such as the exposome – most likely to open up interdisciplinary collaborations remain in practice largely cut off from the social sciences and their research tools. In epidemiological studies (mostly Anglo-Saxon), some characteristics of individuals can even be deliberately treated in an instrumental way [10]. For example, being “white” or “black” is taken as a matter of course a priori, as shown by the racialized variables constantly mobilized by epidemiology. Biomedical research takes these categories as data and does not question them to try to understand what social heterogeneity can cover this clear-cut opposition. And yet, it is recognized that only 15% of the genetic diversity between individuals of the human species is based on differences between groups commonly recognized as “racial”, while the remaining 85% of human genetic diversity is found within racial groups, i.e. between individuals of the “same race” [11].
While the exposome and the environmentalist definition of health on which it is based call on the social and biomedical sciences to interpenetrate, why do the latter ignore the former so radically? Do the social sciences also bear some responsibility for this failed transdisciplinary marriage? This question does not receive a general answer.
2.2. Proposals for collaboration between disciplines: popular epidemiology and environmental justice movements
It should first be recalled that some social scientists have worked on this type of marriage, particularly with the development of “popular epidemiology” [12]. For thirty years, Phil Brown has shown that populations affected by specific health problems (cancer clusters, for example) are subject to local contamination, where “standard” epidemiological studies do not prove conclusive. Working on small samples (a neighbourhood, a street, etc.), this epidemiology involves the populations concerned in the development of field research tools. By collaborating with epidemiologists and social scientists, these residents analyze the occurrence of diseases by highlighting the social factors that can contribute to them: on what empty fields will children play? (This is illustrated in the cover photo of this article.) Do some poor residents recover garbage dumped in a particular place that was previously contaminated with toxic waste? etc.

After founding events (Love Canal [14], Figure 4), and with some tutelary figures from several disciplines, American environmental health research is certainly the one in which the expository and social sciences find themselves discussing most closely, with and thanks to the institutional and financial support of the National Institute of Environmental Health Sciences (NIEHS) [15]. Among other representatives of this interdisciplinarity, we can mention the sociologist Phil Brown who explicitly invites us to go beyond the exposome to develop research that integrates a concept of “socio-exposome” [16] ; but also biologist Rachel Carson, author of the event book Silent Spring, who, as early as 1962, denounced the polluting effects of pesticides and the concealment of their effects by DDT-producing industries; or Sandra Steingraber, also a biologist, whose research claims to be that of an ecologist who originally relied on her own experience of cancer to denounce chemical contamination (Figure 5).


In the cautiously formulated criticism of Fos EPSEAL – a project supported by the Agence Nationale de Sécurité Sanitaire de l’alimentation, de l’environnement et du travail (PNREST Anses, Cancer ITMO AVIESAN, 2014/1/023)… and therefore also by Santé publique France ! -The controversy between standard epidemiological techniques and an interpretation considered to be in favour of exposure and disease prevalence data is never resolved. In a word, the French Public Health report concludes that the results of Fos EPSEAL are of great interest, while indicating that their production methods would benefit from being more clearly stated and more rigorous, and stating that these results are “complementary to the traditional epidemiological approach”. The legitimacy of popular epidemiology is obviously not fully established, despite the euphemisms in the wording… The discussions are in any case not closed, as indicated in a press release dated 20 March 2018, by which the Fos EPSEAL research team takes note of the comments in the French Public Health report, by reviewing the conformity of the survey methods with academic criteria, and by stressing the importance of involving the local populations concerned in the research, so that epidemiological data can also be interpreted through lived experience.

In total, this would describe the gap that remains between disciplinary approaches, despite the research that is attempting to close it:
- On the one hand, research that explicitly mobilizes the notion of exposure is carried out mainly by teams dedicated to life sciences. They can certainly investigate by questionnaire, but in a rather instrumental way, with the final aim of highlighting the molecular signature of exposures in the human body.
- On the other hand, more social science-based approaches, although not necessarily referring to the notion of exposure, develop the study of the social conditions of exposure to toxic substances over the entire – and “locally anchored” – course of people’s lives. Here, the survey by questionnaires and observations is central, and the integration of the approach only exceptionally reaches molecular biology.
With regard to the exposome, it is common to speak of a new “paradigm”, as illustrated by the parliamentary debates on the 2016 Health Act. This suggests that the exposome catalyzes around it a community of researchers and, beyond that, decision-makers who use this notion. But researchers in oomics sciences explain to us that it is difficult to “measure” the exposome and that there is no ideal practical device to make the exposome operational.
To formulate proposals in this sense, we must remember that the sheer size of the technical means does not guarantee that all the mysteries of the diseases hitherto unexplained can be solved. Thus, the socio-demographic variables (e.g. socio-professional categories, age, sex) mobilized in the Global Burden of Disease [21] (GBD), a statistical project of unparalleled historical magnitude, explain only a very small portion of the disability-adjusted life expectancy (“DALYs”) for many chronic diseases (including chronic respiratory diseases). While the same GBD estimates that nearly a quarter [22] of global morbidity, mortality and disability are due to environmental factors, the social characterization of diseases is therefore a blind spot… or almost. In other words, while “the environment” is statistically highlighted as a crucial explanatory factor of health status, this result does not translate into a description of the social characteristics of the populations affected by a particular chronic disease. As if what was described as the “environment” was mysteriously to remain an asocial black box.
The intellectual and philosophical context of North America, which is environmentalist, certainly brings “social scientists” and “biomedical scientists” closer together. But most of them are still sceptical or indifferent about the possibilities of collaborating with the social sciences… and vice versa! However, the situation in countries such as South Africa, which today has a high prevalence of infectious diseases (HIV, tuberculosis) and a growing incidence of diseases of unknown etiology (e.g. autoimmune diseases), is a real challenge for scientific analysis. A challenge that will only be met if each of the disciplines involved takes a step towards its counterparts, towards a truly collaborative and integrated approach to the disciplines. The exposome holds the promise.
Notes and references
Cover image. [Source: Royalty-free image, Pixabay]
[1] https://www.legifrance.gouv.fr/jo_pdf.do?id=JORFTEXT000031912641 (page consulted on August 28, 2017)
[2] Wild C.P. 2005. Complementing the genome with an “exposome”: the outstanding challenge of environmental exposure measurement in molecular epidemiology. Cancer Epidemiology, Biomarkers & Prevention, 14, 8, 1847-1850.
[3] Epidemiology studies, within populations, the statistical distribution of health problems over time and space, as well as the role of the factors that determine them. It is complementary to biomedical sciences that study biological processes.
[4] Techniques for computer analysis of huge datasets.
[5] Wild CP. 2012. The exposome. From concept to utility. International Journal of Epidemiology, 41, 1, 24-32.
Maitre L., de Bont Jeroen, Casas Maribel et al. 2018. Human Early Life Exposome (HELIX) study: a European population-based exposome cohort. BMJ Open, 8: e021311. doi:10.1136/bmjopen-2017-021311
[6] Winslow CEA. 1920. The Untilled Fields of Public Health. Science, New Series, 51, 1306, 23-33.
[7] Poole C, Rothman KJ. 1998. Our conscientious objection to the epidemiology wars. Journal of Epidemiology and Community Health, 52, 10, 613-614. The same could be said of the study of obesity or smoking-related diseases, for example.
[8] Peretti-Watel P. 2004. The use of the epidemiological paradigm for the study of risk behaviours. Revue française de sociologie, 45, 1, 103-132.
[9] Susser M, Susser E. 1996. Choosing a Future for Epidemiology. I. Eras and Paradigms, American Journal of Public Health, 86, 5, 668-673. And: Choosing a Future for Epidemiology. II. From Black Box to Chinese Boxes and Eco-Epidemiology, American Journal of Public Health, 86, 5, 674-677.
[10] Shim JK, Weatherford Darling K, Lappe MD, Thomson LK, Soo-Jin Lee S, Hiattt RA, Ackerman SL. 2014. Homogeneity and heterogeneity as situational properties: Producing – and moving beyond? – race in post-genomic science. Social Studies of Science, 44, 4, 579-599.
[11] Lewontin Richard. 1972. The apportionment of human diversity in Theodosius Dobzhansky, Max K. Hecht, William C. Steere (eds.), Evolutionary Biology, Volume 6. New York: Appleton-Century-Croft, 381-398.
[12] Brown P. 1992 Popular epidemiology and toxic waste contamination: lay and professional ways of knowing, Journal of Health and Social Behavior, 33, 3, 267-281.
[13] Brown P., Morello-Frosch R, Zzavestoski S and the Contested Illnesses Research Group (eds.). 2012. Contested Illnesses. Citizens, Science and Health Social Movements. Berkeley, LA, London: University of California Press.
[14] https://www.justice.gov/enrd/us-v-occidental-chem-corp (page consulted on October 12, 2018)
[15] Hoover E, Renauld M, Edelstein MR, Brown P. 2015. Social Science Collaboration with Environmental Health. Environmental Health Perspectives, 123, 11, 1100-1106.
[16] Senier L., Brown P., Shostak S., Bridget H. 2017. The socio-exposome: advancing exposure science and environmental justice in a postgenomic era. Environmental sociology, 3, 2, pp. 107-121.
[17] Chaumel M., La Branche S. 2008. Ecological inequalities: towards which definition? Espaces, populations et sociétés, 1, p. 101-110. Larrère C (dir.). 2017. Environmental inequalities. Paris: PUF, La Vie des idées.
[18] https://f-origin.hypotheses.org/wp-content/blogs.dir/3282/files/2017/01/FOS-EPSEAL-ANSES-16-1-2017-logo-red.pdf (page consulted on October 12, 2018).
[19] http://invs.santepubliquefrance.fr/Publications-et-outils/Rapports-et-syntheses/Environnement-et-sante/2018/Rapport-d-analyse-de-l-etude-Fos-Epseal (page consulted on October 12, 2018).
[20] See Canguilhem G. 2009[1952]. La connaissance du vivant, Chapter III: “Le vivant et son milieu”, p. 165-197. Paris: Vrin (Bibliothèque des textes philosophiques).
[21] GBD 2013 DALYs and HALE Collaborators. 2015. Global, regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990-2013: quantifying the epidemiological transition. The Lancet, 386, 2145-91.
[22] Prüss-Ustün A, Wolf J, Corvalán C, Bos R, Neira M. 2016. Preventing disease through healthy environments. A global assessment of the burden of disease from environmental risks. Geneva?
The Encyclopedia of the Environment by the Association des Encyclopédies de l'Environnement et de l'Énergie (www.a3e.fr), contractually linked to the University of Grenoble Alpes and Grenoble INP, and sponsored by the French Academy of Sciences.
To cite this article: CAVALIN Catherine (February 11, 2019), Exposome and social sciences: the promise of a meeting?, Encyclopedia of the Environment, Accessed November 21, 2024 [online ISSN 2555-0950] url : https://www.encyclopedie-environnement.org/en/society/exposome-social-sciences-promise-of-meeting/.
The articles in the Encyclopedia of the Environment are made available under the terms of the Creative Commons BY-NC-SA license, which authorizes reproduction subject to: citing the source, not making commercial use of them, sharing identical initial conditions, reproducing at each reuse or distribution the mention of this Creative Commons BY-NC-SA license.