Acute stress, chronic stress, stress management methods in humans
PDF
The term “stress” is used to describe an unpleasant relationship with events in our daily lives. Some people are able to cope with it, while others find it more difficult, or are even overwhelmed by these reactions. But in biological terms, what is stress? How does our body respond to stress? Are there ways of reducing its impact on our bodies? To limit the deleterious effects of stress, it is therefore important to implement treatments, both medicated (e.g. β-blockers) and non-medicated (e.g. cognitive-behavioural therapies).
- 1. History and definition(s) of stress
- 2. Stress response effectors
- 3. Stressful stimuli, different responses
- 4. Acute stress, chronic stress
- 4.1. The 1st bomb is linked to corticoid hypersecretion.
- 4.2. When hippocampal networks are impaired, all cognitive functions may be affected: this is the 2nd bomb.
- 4.3. The 3rd bomb is linked to the effect of stress on the immune system [14].
- 4.4. The 4th bomb involves modifications of an epigenetic nature.
- 5. Stress management methods
- 6. Messages to remember
1. History and definition(s) of stress
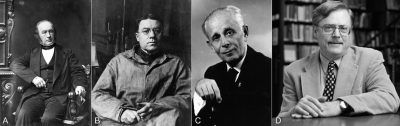
Historically, several major physiologists have contributed to the development of stress-related concepts [1] (Figure 1). Walter Bradford Cannon (1871-1945) studied visceral adaptations to certain stimuli, particularly nociceptive ones. He showed that an animal faced with an aversive situation, such as the presence of a competitor in its territory or an encounter with a predator, responds with two possible behaviors: defense with withdrawal or attack. These behavioral manifestations are accompanied by metabolic changes that mobilize the organism’s reserves. Cannon based his concept of homeostasis on the work of Claude Bernard (1813-1878) on the internal environment and, in the light of this work, renamed the observed responses “fight or flight“.
Hans Selye (1907-1982) took up and continued these studies by working on the general adaptation syndrome. He systematized the description and showed that it consists of three stereotyped phases, whatever the aversive situations in which the individual is placed: phases of alarm, resistance and then exhaustion when the stimulus is maintained.
- The alarm phase is the body’s first line of defense in response to changes in its environment, and is currently referred to as the “acute response” to stress.
- The resistance phase corresponds to the regulations brought into play when the stress situation becomes chronic.
- Finally, the exhaustion phase occurs when regulatory systems are overwhelmed and pathologies set in.
Selye also showed that injecting animals with an adrenal extract reproduced the effects of the general adaptation syndrome. The main substance responsible for this effect has since been purified: a glucocorticoid [2], cortisol. Finally, he proposes a generalization of the definition of stress: “a non-specific response of the organism to any demand made upon it“.
Work on characterizing the mechanisms of response to stressful stimuli continued throughout the 20th century. In particular, Bruce McEwen (1938-2020) documented the involvement of glucocorticoid receptors in this response. The body’s adaptation mechanisms are now better understood, and a consensus has emerged on the current definition of stress as “the response to an event that disturbs an individual’s internal environment, leading to the activation of regulatory mechanisms that serve to restore homeostasisIn biology and systems, homeostasis is a phenomenon whereby a key factor (e.g. temperature) is maintained around a value that is beneficial for the system in question, by means of a regulatory process. Typical examples of homeostasis are: the temperature of a room controlled by a thermostat, the body temperature of a homeothermic animal, the blood sugar level, the degree of acidity of an environment, the internal pressure of an environment, and so on. More generally, homeostasis refers to a system’s overall ability to maintain a set of key factors, particularly in a living organism.” [3].
2. Stress response effectors
2.1. Regulatory loops for handling stressful situations
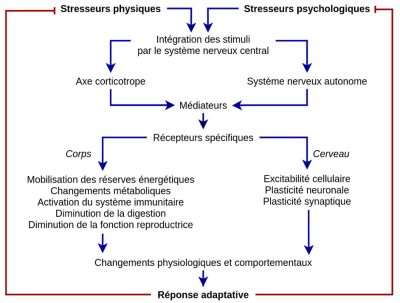
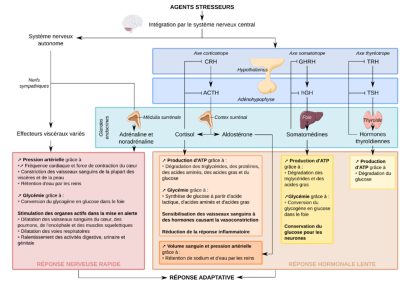
Stressors can be divided into two categories: psychological and physical. Their analysis and processing by the central nervous system will differ (see below), but will ultimately lead to the development of the stress response, which involves the hypothalamic-pituitary-adrenal axisThe hypothalamic-pituitary-adrenal axis is formed by the hypothalamus, the pituitary gland and the adrenal gland, which releases hormones such as cortisol (the stress hormone). It links the central nervous and endocrine systems. It is at the heart of the biological responses of stress and resilience, together with the autonomic nervous system and the behavioural processes of adaptation. (or corticotropic axis) and the autonomic nervous system. The mediators released during this response act on specific receptors in the central nervous system, as well as throughout the body, to produce physiological and behavioral responses that enable the body to adapt to its new environment. This complex response manifests itself in the mobilization of energy reserves, metabolic changes, activation of the immune system, limitation of digestive processes, reduced fertility and reproductive behavior. These different elements are the result of genomic and epigenetic regulations that modify cellular functioning, and of non-genomic controlsRegulation involving intracellular “second messenger” signalling pathways. [4] resulting in changes in cellular excitability, as well as neuronalThe expression “neuronal plasticity” is a generic term that describes the mechanisms by which the brain is capable of modifying itself during the processes of neurogenesis from the embryonic phase or during learning. and synaptic plasticityThe expression “synaptic plasticity” refers to the ability of synapses to modulate the efficiency of the transmission of an electrical signal from one neuron to another following a particular event – a one-off significant increase or decrease in their activity – and to retain a “trace” of this modulation over time. [1].
2.2. An example: escape from a predator
When an individual is confronted with a predator, the response that is triggered is a stereotyped behavior known as “escape behavior”. To be effective, the escape response requires the prey to be able to run long enough, fast enough and avoid obstacles. It is the effectors – the autonomic nervous system and the corticotropic axis – that enable this coordinated, effective and long-lasting response.
- Oxygen and nutrient supply
Long-distance running requires muscular contractions in an aerobic regime, and therefore a sufficient supply of O2 and nutrients to the skeletal muscles of the limbs. This is made possible by changes in the blood flows perfusing the various organs. While blood flow decreases in the digestive tract, it increases in the skeletal muscles involved, thanks to vasodilatation of the arterioles irrigating them. In the body as a whole, accelerated heart rate increases cardiac output, and increased respiratory rate increases O2 supply to the cells. All these functional adaptations, both cardiovascular and respiratory, are under the control of the orthosympathetic autonomic nervous system, of which noradrenaline is the final neurotransmitter. Adrenalin, secreted by the adrenal medulla when stimulated by the sympathetic nervous system, is also a major player in these control systems.
- Mobilization of body reserves
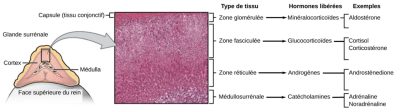
Metabolic support for this active race is provided by mobilizing the body’s reserves. Indeed, muscle glycogen stores are not sufficient to ensure long-lasting contractile muscular activity. Other reserves, such as liver glycogen or triglycerides from adipose tissue, are then brought into play, enabling muscle cells to produce sufficient ATP. The adrenal glands in particular (Figure 3) are involved in this mobilization of energy reserves: the cortical part as part of the corticotropic axis (secretion of glucocorticoids) and the medullary part under the control of the autonomic nervous system (secretion of adrenalin).
When the stressor stimulus is maintained for longer, the metabolic response may be sustained by the later activation of the somatotropic and thyrotropic axes [5], whose hormones also exert metabolic effects (Figure 4).
- The body’s reactivity and increased vigilance
2.3. Temporal sequence of effector system activation
The two effector systems, the autonomic nervous system and the corticotropic axis, operate with different response kinetics. The first, nervous, is a fast effector, ensuring the initial actions of the escape behavior, while the second, hormonal, is a slower effector, maintaining motor and metabolic responses for the duration of the escape behavior. Moreover, as glucocorticoids are hormones that activate transcription factors, their effects take longer to take effect than those of hormones acting via membrane receptors.
The coordinated and successive activation of the autonomic nervous system and the corticotropic axis (or even other endocrine axes) is ensured by the hypothalamus. This small diencephalic brain structure, about the size of an almond in humans, plays the fundamental role of “conductor of vegetative life” (Figure 5), and thus of the stress response. It receives activations induced by stressful stimuli via the various sensory and decision-making brain structures afferent to it. It projects onto the brain stem, which contains the control centers of the autonomic nervous system and, together with the pituitary gland, forms the hypothalamus-pituitary complex that regulates the activity of most endocrine glands. The hypothalamus is thus positioned at the crossroads of afferent and efferent pathways, enabling it to fulfill its integrative role.
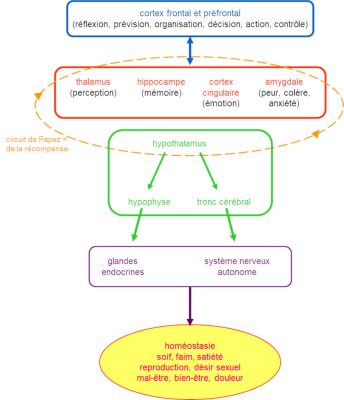
3. Stressful stimuli, different responses
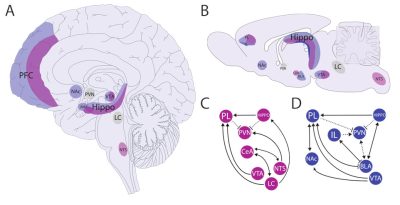
This third section looks at how stressful stimuli are processed centrally to trigger the stereotyped effector response [1]. Several brain areas are involved. Cognitive processing is carried out by the prefrontal cortex, which is highly developed in primates. The amygdala and the reward circuit [6] (including the nucleus accumbens in the striatum and the ventral tegmental area in the midbrain) enable an aversive component to be associated with stressful events. Finally, the hippocampus is involved in learning and memory processes. These different brain areas are connected, directly or indirectly, to the hypothalamus, which triggers the peripheral effector response via the brainstem and the hypothalamo-hypophyseal complex (Figure 5).
Depending on the nature of the stressful stimulus, whether physical or psychological, the central nervous system processes it differently: a painful stimulus generates a rapid motor response (the essentially spinal withdrawal reflex), whereas a stimulus that is more difficult to bear psychologically, or a mixed stimulus combining physical and psychological pain, gives rise to a more complex response, combining cognitive elements and motor events (Figure 6) (read Focus on Stressor processing networks)
Physical stressors are processed primarily at the level of the brainstem and hypothalamus, with little activation of the limbic system [7] (amygdala, hippocampus, prefrontal cortex) and very little interaction with the reward circuit, which shows little electrical activity in these situations.
For psychic stressors, the physical and cognitive response strongly involves the limbic system (in particular the prefrontal cortex) and the reward circuit, which are interconnected and contribute to the complex manifestations linked to the stressful event. The prefrontal cortex develops an appropriate response strategy to environmental changes.
The hippocampus, a brain structure involved in learning, activates or inhibits the corticotropic axis according to the inputs it receives. In response to stress, glucocorticoid receptors, expressed in large quantities in the hippocampus and hypothalamus, are occupied, which modifies the connectivity of the neuronal networks that make them up, inducing synaptic elasticity, the substrate of learning and sensitization. Thus, if a stressful situation arises again, the individual is able to progress and cope more easily [8].
Other brain structures are also involved in the response to a stressful event. The amygdala processes emotions and consolidates memories linked to the stressful event, in association with the hippocampus. The nucleus accumbens receives projections from the hippocampus, which help increase sensitivity to psychological stress, projections from the amygdala, which are involved in feelings of reward (or “punishment”), and projections from the prefrontal cortex, which are involved in the resilience process [9]. Thus, the reward circuit is a key system for the elaboration of aversive mechanisms (avoidance, anhedonia) [1].
As already mentioned for glucocorticoids, receptors for stress mediators (adrenalin, noradrenalin, corticoids, CRH, etc.) are expressed in the central nervous system, notably in the nuclei involved in stress management. By binding to their receptors, these mediators, produced by peripheral organs, in turn modify the activity of brain nuclei. This feedback system, typical of homeostatic processes, helps to deal with the stressful stimulus [10].
4. Acute stress, chronic stress
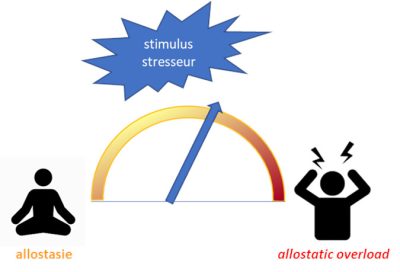
This imbalance may set in immediately or, more insidiously, over a long period of time. It is at the origin of several “bombs“, due to the exacerbation of the processes seen above, which can generate or reveal various pathological states, and can even, at least in rodents, be transmitted to subsequent generations via epigenetic mechanisms.
4.1. The 1st bomb is linked to corticoid hypersecretion.
As we have seen, the hippocampus is a structure with a high density of glucocorticoid receptors. Their massive activation leads to alterations in neurogenesis (the hippocampus contains stem cells involved in the formation of new memories [12]) and synaptic transmission. The resulting high release of glutamate can induce excitotoxicity [13] of neurons and glial cells, which can lead to profound dysfunction of this brain structure [14].
4.2. When hippocampal networks are impaired, all cognitive functions may be affected: this is the 2nd bomb.
Dysfunction of the hippocampal networks has repercussions on the structures responsible for cognition, resulting in impaired attention and cognitive flexibility, which are essential for learning and adapting to stressful situations. This dysfunction also modifies reward and aversion behaviours, leading to a loss of the hedonic value of certain stimuli [11].
4.3. The 3rd bomb is linked to the effect of stress on the immune system [14].
Depending on the situation and the regulatory pathway involved, corticoids can have a stimulatory or inhibitory effect on the inflammatory and immune response. If corticoid secretion is exacerbated, immune system regulation can lead to peripheral and central disorders, as the immune, nervous and endocrine systems are interconnected. For example, activation of microglial cells induces inflammation in nervous tissue, disrupting the activity of neuronal networks.
The chronicity of the stressful stimulus has an aggravating effect, and these various events could be at the root of neuropathologies such as depression, fatigue, chronic pain, cognitive impairment, but also peripheral pathologies such as altered immune response (particularly T-cell response) and metabolism (such as insulin resistance or osteoporosis) [15].
4.4. The 4th bomb involves modifications of an epigenetic nature.
The modifications we have just mentioned affect the expression of various genes, such as the one encoding the glucocorticoid receptor, those encoding certain transcription and growth factors, or genes linked to neurotransmission (for example, that of POMC, precursor of ACTH, but also of β-endorphins, neurotransmitters involved in the control of pain pathways).
Beyond modulating gene expression, these modifications can also affect the epigenome, with lasting consequences. Such epigenetic modifications constitute a substrate of vulnerability and can be transmitted to offspring. This has been demonstrated, for example, in rodents, where separation of the young from their mother for a short time (a few minutes a day) results in an increased susceptibility of the juvenile to opiate intake [16],[17].
These different “bombs” are found when analyzing pathologies with a stress-related component, such as chronic fatigue syndrome, burnout, post-traumatic stress states, neglect in early childhood… They can also aggravate multifactorial pathologies following imbalance of the corticotropic axis, such as anxiety states, depressive states, epilepsy, cardiovascular diseases, diabetes, etc. They are then not triggered by the stress-related component, but by the stress-related component. They are not triggered by a stressful event, but the stressful environment may contribute to their development or reveal them.
5. Stress management methods
Generally speaking, stress management methods follow the following pattern: assessment of the stressful situation, then development of the ability to cope with it in order to avoid reaching a pathological state. These methods call on a therapeutic arsenal of two non-exclusive types: a medicinal approach or psychotherapeutic treatment [18] (Table 1).
Table 1. The different methods of stress management. Author(s)/Author(s): Hélène Hardin-Pouzet
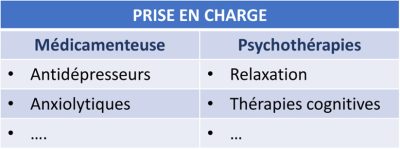
5.1. Pharmacological methods
These target the various effectors of the stress response. Historically, glucocorticoid receptor antagonists [19] or cortisol synthesis inhibitors have been prescribed, but these have numerous side effects. Currently, selective glucocorticoid receptor modulators (SGRMs) are being studied, but their efficacy has yet to be increased. This approach to modulating the corticoid pathway is extremely complex, due to the intertwining of the synthesis pathways of the different steroids.
Other molecules are used for stress management purposes, notably those acting on catecholaminergic transmission [20]. This is the case with β-blockers (propranolol), but their side effects, particularly on heart rate, are not negligible. This is also the case with catecholamine synthesis or reuptake inhibitors, but here again their side effects are significant (cf. amphetamines and Mediator). Finally, indirect pharmacological treatments targeting stress-related disorders can be proposed: these include antidepressants or anxiolytics that act on serotonergic or GABAergic transmission.
5.2. Non-drug treatment
This aims to reconstruct the behavioral response chain in order to regain a homeostatic state and establish a state of resilience. Several techniques can be proposed [21].
Relaxation provides neuromuscular relaxation, reducing anxiety-related tension and achieving inner calm, while cognitive behavioral therapies train the individual to respond in a controlled way to the stressful situation. Behavioral therapies re-expose the individual briefly to the stressful situation, or to its memory, then gradually increase the intensity of the stress in order to overcome it. In this respect, virtual reality tools can be useful, particularly when working with certain phobias [22].
Cognitive therapies take a different approach: they involve developing a cognitive restructuring process that enables negative thoughts to be left behind and replaced by positive ones, in order to overcome the stressful situation. These approaches have been used to treat certain cases of post-traumatic stress disorder. For example, one study showed the beneficial effects of music therapy through MRI monitoring and the measurement of certain biological parameters [23],[24]. Meta-analyses have also shown improvements in anxiety and depressive symptoms in a cohort of students practicing meditation sessions [25].
6. Messages to remember
- A stressor is a stimulus of physical or psychological origin that disturbs the body’s state of equilibrium.
- The response to a stressor is known as acute stress and, via the corticotropic (or hypothalamic-pituitary-adrenal) axis and the autonomic nervous system, enables a new state of equilibrium to be established, known as allostasis.
- When the stressful situation is too intense or lasts too long, allostasis cannot be achieved, and chronic stress can then be the cause of certain pathologies, reveal underlying pathologies, or even have an impact on subsequent generations.
- To limit the deleterious effects of stress, it is therefore essential to implement treatments, whether medicinal (e.g. β-blockers) or non-therapeutic (e.g. cognitive-behavioral therapies).
This article was originally published in December 2021 by Planet Vie under Creative Commons license: Acute stress, chronic stress, stress management methods in humans. It was edited by Pascal Combemorel, Planet-Vie’s Editorial Manager.
Notes and references
Cover image. [Source: CIPHR Connect, CC BY 2.0 <https://creativecommons.org/licenses/by/2.0>, via Wikimedia Commons]
[1] L. D. Godoy, M. T. Rossignoli, P. Delfino-Pereira, N. Garcia-Cairasco, &E. H. de Lima Umeoka, “A ComprehensiveOverview on Stress Neurobiology: Basic Concepts and Clinical Implications,” Front BehavNeurosci, vol. 12, p. 127, 2018, doi: 10.3389/fnbeh.2018.00127.
[2] Corticoids (or corticosteroids) are a class of hormones derived from cholesterol. They are synthesized by the cortex of the adrenal glands. Glucocorticoids are produced by the fasciculated zone of the adrenal cortex. They act on carbohydrate metabolism and have an anti-inflammatory effect. The glucocorticoids produced by the adrenal glands are cortisol (the main glucocorticoid in humans), and/or corticosterone (the main glucocorticoid in rodents). Cortisone, actually hydrocortisone, which is used therapeutically, has no direct biological activity: it must be metabolized by the liver into cortisol to be effective.
[3] Fink G. Ed. 2000, “Encyclopedia of Stress – 1st Edition”. eBook ISBN:9780080569772.
[4] By “genomic regulations” we mean controls that modulate gene expression (via transcription factors), by “epigenetic regulations” we mean regulations that act on genome expression without altering its nucleotide sequence (DNA methylation, post-translational modifications of histones, etc.) and by “non-genomic controls” we mean regulations involving intracellular, “second messenger” type signalling pathways.
[5] The function of the somatotropic axis is to control the body’s growth via growth hormone (GH) and somatomedin (IGF-1), which supply cells with nutrients and control the rate of cell division. The thyrotropic axis controls production of the thyroid hormones T3 and T4, which have pleiotropic effects, including on cell metabolism.
[6] Tassin, J.P., 2021, Le circuit de la récompense. Planet Vie.
[7] The limbic system corresponds to a set of cortical and subcortical structures involved in emotions.
[8] On the other hand, if the individual is unable to cope with the repetition of the same stressful event, stress becomes chronic (see next section).
[9] Resilience is the ability to overcome a traumatic event and no longer be affected by it.
[10] M. Joëls and T. Z. Baram, “The neuro-symphony of stress”, Nat RevNeurosci, vol. 10, no. 6, pp. 459-466, June 2009, doi : 10.1038/nrn2632.
[11] P. Boucher and P. Plusquellec, “Acute Stress AssessmentFrom Excess Cortisol Secretion: Fundamentals and Perspectives,” Front Endocrinol (Lausanne), vol. 10, p. 749, 2019, doi: 10.3389/fendo.2019.00749.
[12] A. Gros, “Adult neurogenesis in mammals”, Planet-Vie, 2018 (access March 3, 2023)
[13] Glutamate is the main excitatory neurotransmitter of the central nervous system. It acts via calcium channel receptors on neurons and glial cells. When released in large quantities, it causes massive excitation of these cells, leading to their destruction.
[14] M.-P. Moisan and M. Le Moal, “[Overview of acute and chronic stress responses]”, Med Sci (Paris), vol. 28, no. 6-7, pp. 612-617, Jul. 2012, doi: 10.1051/medsci/2012286014.
[15] I. H. Jonsdottir and A. SjörsDahlman, “MECHANISMS IN ENDOCRINOLOGY: Endocrine and immunological aspects of burnout: a narrative review”, Eur J Endocrinol, vol. 180, no. 3, pp. R147-R158, March 2019, doi: 10.1530/EJE-18-0741.
[16] C. Tesone-Coelho et al, “Vulnerability to opiate intake in maternally deprived rats: implication of MeCP2 and of histone acetylation”, Addict Biol, vol. 20, no. 1, pp. 120-131, Jan. 2015, doi: 10.1111/adb.12084.
[17] M. Rincel et al, “Environnement précoce et vulnérabilité neuropsychiatrique”, Med Sci (Paris), vol. 32, no. 1, Art. no. 1, Jan. 2016, doi: 10.1051/medsci/20163201015.
[18] “ALD n°23 – Troubles anxieux graves“, Haute Autorité de Santé.
[19] Like RU486, the active ingredient in the morning-after pill, but initially developed for its glucocorticoid receptor antagonist action.
[20] Catecholamines are molecules characterized by the presence of a catechol nucleus (a benzene nucleus with two adjacent alcohol groups) associated with an amino side chain. In the context of stress, the two main catecholamines are noradrenalin and adrenalin.
[21] “Anxiete.fr : le site de référence de l’anxiété“, Anxiété.
[22] A. S. Rizzo, S. T. Koenig, and T. B. Talbot, “Clinical Virtual Reality: Emerging Opportunities for Psychiatry,” Focus (Am PsychiatrPubl), vol. 16,no. 3, pp. 266-278, Jul. 2018, doi: 10.1176/appi.focus.20180011.
[23] A. Witusik and T. Pietras, “Music therapy as a complementary form of therapy for mental disorders”, Pol MerkurLekarski, vol. 47, no. 282, pp. 240-243, Dec. 2019.
[24] A. Witusik, K. Sipowicz, M. Podlecka, and T. Pietras, “Music therapy and psychotherapy as non-pharmacological methods supporting therapy in medicine – similarities and differences,” Pol MerkurLekarski, vol. 48, no. 284, pp. 139-142, Apr. 2020.
[25] G. González-Valero, F. Zurita-Ortega, J. L. Ubago-Jiménez, and P. Puertas-Molero, “Use of Meditation and Cognitive Behavioral Therapies for the Treatment of Stress, Depression and Anxiety in Students. A Systematic Review and Meta-Analysis”, Int J Environ Res Public Health, vol. 16, no. 22, p. E4394, Nov. 2019, doi: 10.3390/ijerph16224394.
The Encyclopedia of the Environment by the Association des Encyclopédies de l'Environnement et de l'Énergie (www.a3e.fr), contractually linked to the University of Grenoble Alpes and Grenoble INP, and sponsored by the French Academy of Sciences.
To cite this article: HARDIN-POUZET Hélène (May 11, 2024), Acute stress, chronic stress, stress management methods in humans, Encyclopedia of the Environment, Accessed November 24, 2024 [online ISSN 2555-0950] url : https://www.encyclopedie-environnement.org/en/health/acute-stress-chronic-stress-stress-management-methods-in-humans/.
The articles in the Encyclopedia of the Environment are made available under the terms of the Creative Commons BY-NC-SA license, which authorizes reproduction subject to: citing the source, not making commercial use of them, sharing identical initial conditions, reproducing at each reuse or distribution the mention of this Creative Commons BY-NC-SA license.