空气颗粒物及其健康效应

空气颗粒物是主要的大气污染物之一,其主要健康效应多年来已为人知。已有大量研究开展空气颗粒物对死亡率、肺及心血管并发症发生的影响,表明其对人体的长期效应比短期效应更严重。尽管空气颗粒物污染物造成了相当大的社会经济损失,但相应的预防措施仍然不足。
1. 一般概念
每个人都需要呼吸才能生存,因此空气质量极为重要。不同于其它暴露途径(如食品),没有人可以不呼吸,因此空气质量才备受人们关注,无论老少,健康与否。对空气污染的健康效应研究已持续了几十年之久。自1930年比利时默兹河谷事件首次引起警示,以及1952年12月伦敦烟雾事件造成了数千人的死亡后,人们已对不同空气污染物的人体健康效应有了更深刻的认识。
空气中存在许多自然源或人为源的污染物,其中悬浮颗粒一直是研究的焦点。
1.1 悬浮颗粒
空气颗粒是来自于不同颗粒排放源的复杂混合物,既含有机组分,也含无机组分。目前,仍然无法对颗粒的不同组分进行常规、精确地区分(见空气污染颗粒:它们是什么?)。因此,除非在实验室严格控制的实验条件下,否则不可能厘清颗粒特定成分的健康效应。因此,在人群水平上观测到的健康效应主要归因于颗粒物的总体效应,无法区分某种具体成分的效应。
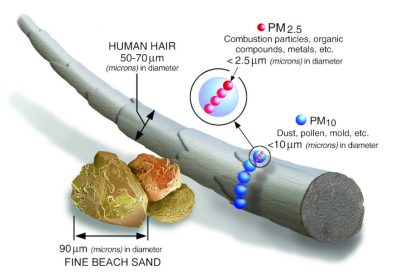
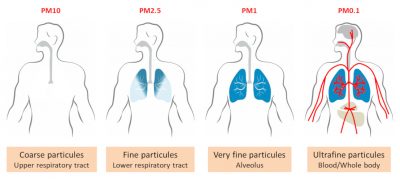
颗粒物 (PM) 按其空气动力学直径(微米)进行分类。在法国,空气质量监测设备常规分析的颗粒物包括:直径为10微米的颗粒物,被称为PM10或“粗”颗粒;直径小于等于2.5微米的颗粒物(PM2.5),被称为“细”颗粒(见图1);近年来,直径小于等于0.1微米(100纳米,即PM0.1或纳米颗粒)的“超细”颗粒引起了科学家的广泛兴趣。
颗粒直径至关重要,因为它决定了颗粒穿透支气管肺系统并进入人体的状态(见图2)。事实上,只有PM2.5及直径更小的颗粒物才能深入到肺部并进入肺泡。部分PM0.1甚至能穿透将空气与血流分开的肺泡毛细血管膜进入体内。人体内的真实情况可能更加复杂,仍未被完全认知。对这方面的大部分认识主要来源于数学模型和一些动物实验。
颗粒进入人体的其他途径还包括消化系统和皮肤。摄入被颗粒污染的食物和饮料,以及沿支气管上皮运输过程中从气管支气管枝中排出的颗粒,都会产生颗粒的消化渗透。目前,厘清颗粒摄入和消化道疾病之间的联系还为时尚早,相关研究的结论并不一致[1]。类似地,皮肤途径也仍然需要更多的研究,才能获得定论。常规空气PM10浓度的测量包括两种方式:一种由靠近或距离排放源一定距离的固定的空气质量分析站测量,通常在工业生产设备周边、城区内或道路轴线附近;另一种是距已知排放源一定距离,即能检测可能的污染峰值,也能测量“背景噪音”。通常,移动监测站(见图3)也可用于远离排放源的现场空气分析。细颗粒物(PM2.5和PM0.1)的常规测量还没有,但对PM2.5的分析在不断增多。

毫无疑问,空气质量的改善尤其需要减少人为排放。但常令人费解的是,污染物排放浓度和大气污染物浓度之间存在差异。空气质量的参考依据有时是根据颗粒物(或污染物)的排放浓度,有时是根据大气中颗粒物(或污染物)的浓度,这使如何改善空气质量变得复杂起来。当我们谈及污染物排放,我们从根本上就把污染物和其可能带来的健康影响联系起来。根据各部门(如公路运输、工业、供暖)提供的排放量(按公斤计算)数据,我们能估算出每个部分的贡献值,但是大气中的颗粒并不具其来源特征(需要具体分析)。换句话说,污染物排放浓度和大气污染物浓度并不是同一个概念,这就解释了为什么估算的排放污染物浓度和测量的大气污染物浓度的时间趋势会明显不同。例如,2000年至2010年间的法兰西岛,PM10的排放量下降了41%,但同期大气中PM10的浓度仅下降了7%。因此,降低污染物排放量势在必行,但这并不意味着大气中污染物浓度会同比下降。同时,风和大气湍流还可能影响污染物(特别是细颗粒物和超细颗粒物)的远距离传输。因此,乡村的空气并不总是优于城市。
因此,降低污染物排放量势在必行,但这并不意味着大气中污染物浓度会立竿见影的同比例下降,因为风和大气湍流还影响污染物(特别是细颗粒物和超细颗粒物)的远距离传输。因此,乡村的空气并不总是优于城市的空气。
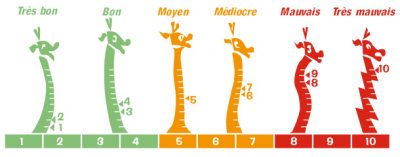
大气指数(AMTO index,图4)是法国采用的判断空气质量的综合指标(分为1-10级),汇总了四种主要污染物(硫氧化物、氮氧化物、臭氧、PM10)的持续分析,被应用于居住人口超过10万的所有城市。最高分即为四种污染物浓度最高的那一种。任何人都能在互联网上公开查询到各城镇的大气指数(例如ATMO Auvergne Rhône-Alpes)。官方机构可利用大气指数向公众发布通知或警报。空气质量指数(AQI)是大气指数的简化版。
因此,大气指数能用于监测污染峰值,如在冬季高压期常出现的PM10峰值,或盛夏期间的臭氧峰值。另一方面,这可能也带来误解,即暗示公众或特定官方机构只有当污染达到峰值时健康才受到威胁。然而,如我们所知,不仅在污染高峰期,大气颗粒物的长期暴露也会影响健康。因此,污染高峰只是空气污染影响健康的冰山一角!
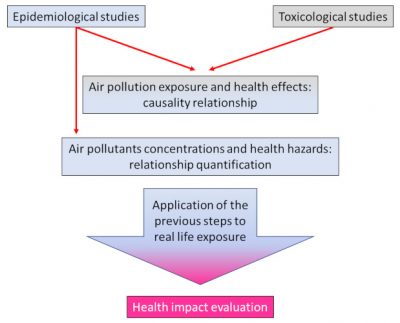
1.2 如何研究颗粒物的健康效应?
毒理学使得利用数学或实验模型,在细胞、组织或动物水平研究污染物对健康的影响成为可能。在严格的条件下,可研究特定污染物对某一器官的影响,即开展风险评估。风险评估是通过研究和量化我们的暴露物(暴露场景),最终比较实验室测量的风险水平与真实暴露的风险水平。基于这些研究,科学家向当局提出健康的“标准”,即通常不应超过的浓度阈值。
当在实验室中可检测到出现效应的阈值时,“建立”标准相对简单。通过纳入一系列“不确定因素”后,便能够提出适用于人类的“阈值”,即标准。更为复杂的情况是,当物质在最低剂量也体现出毒性时,便无法获得阈值。这种情况适用于大部分空气污染物,包括颗粒物。因此,就空气质量而言,“监管”标准即为通过模拟“可接受”风险而估算得到的浓度阈值。这些标准总被视为暂定的、可能是“最不糟糕”的。因为我们必须呼吸,所以零风险是不存在的[2]。
流行病学,即研究潜在影响因素与疾病的频率、分布和演变间联系的学科,可评估空气污染在人群、城市、地区和国家等范围的影响[3]。流行病学主要采用时间序列和队列研究两种方法来研究空气污染的健康效应。
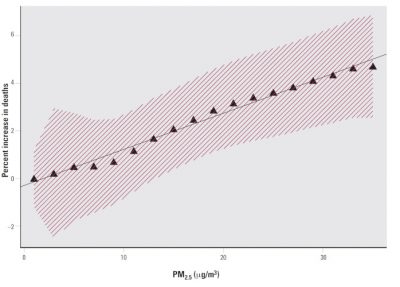
时间序列试图在一段时间内(相对短的时间周期),建立空气污染与死亡人数、入院人数、药品消费量、心肺疾病频率等之间的联系(见图5)。尽管长期以来污染峰值一直是关注的焦点,但自20世纪90年代以来,时间序列使得观测污染的每日波动对健康的影响成为可能。时间序列的优势之一在于,在相对较短的周期内或不同周期间,可观测同一人群,这可以有效消除许多混杂偏倚,例如在一段时间内基本没变化的吸烟、医疗或社会经济状况等[4]。另一方面,必须得考虑所有具有快速动力学的现象,如流感流行或短期天气变化。
队列研究可提供长期、多年的结果。队列指符合特定条件并被随时观测的人群。队列研究常包括大量人数,如数千人,对他们的习惯、隐私、职业环境和医疗状况等进行多年跟踪,并记录其在研究期间的所有活动,如发病情况等。这种所谓的前瞻性研究需要投入大量人力和财力。
也可进行其他类型的研究,如病例对照研究或病例交叉研究,均属于回顾性研究。病例对照研究,旨在对比患病个体与健康个体,寻找一种或更多因素解释疾病。案例交叉研究,旨在通过个体观测,解释随时间发生的变化。针对空气污染的研究,考虑到各种观测到的人体效应,病例对照研究或病例交叉研究不如队列研究可靠,并不常见。
流行病学使得测量“相对风险”成为可能,即处于风险个体的发病率与无风险个体的发病率间的联系。发病率为给定时期(如一年)内疾病新增病例的频率。我们这里讨论的是高风险和低风险。例如,主动吸烟的相对风险在30左右,即吸烟者发生肺癌的几率比不吸烟者发生肺癌的几率高30倍。空气污染被认为是“低”风险,相对风险小于2。重要的是要理解,尽管空气污染导致健康效应发生的几率较低,然而一旦发生,后果可能同样严重。健康效应的低发生率解释了队列研究必须囊括数以千计的个体进行观测,以获得有意义的结果。
最终,统计学方法被应用于所有病例,旨在排除任何偶然因素带来的结果。假设我们想研究空气污染对所有法国人的健康效应,能否通过跟踪6600多万人若干年,进行队列研究呢?当然不能。因此,常选择具有多样性组成的人群作为 “代表性”样本,结合统计学方法来验证获得的结果。统计检验使得建立空气污染和健康效应间的“显著”关联性成为可能。然而,有必要建立的是颗粒物和健康效应间真正的因果关系[5],而非简单的统计相关性[6]。正如Dab等人在2001年[7]所讨论的,大多数现有研究的方法学允许建立这种因果关系。最常用的标准[3]包括:一致性和重现性,即效应是不变且可重现的;时效性,即暴露-时间的效应是一致的;剂量-反应的效应(取决于毒性物质)和生物学合理性,即已知毒性机制与观测到效应的一致性。
2. 作用机制
细胞水平和动物体内的毒理学研究有助于更好理解颗粒对人体的作用机制,并能在很大程度上解释流行病学研究所论证的颗粒物与健康效应之间的相关性[8]。
细颗粒和超细颗粒可以在肺泡中沉积,被称为可吸入颗粒物。已有研究表明,阻塞性支气管疾病(如哮喘和慢性阻塞性支气管病)患者的肺部颗粒物沉积量更高。颗粒物在肺部区域的沉积具有异质性,且个体差异很大。小部分超细颗粒能够进入血液,进而到达其它器官[9]。
另外,超细颗粒的另一个到达大脑的潜在途径是嗅通路[9]。如前所述,针对颗粒物的消化和皮肤渗透途径的研究还不充分,存在相互矛盾的结果。
颗粒的致病性由其粒径、化学组分、来源、溶解度和生产活性氧的能力决定。颗粒的化学组分差异很大,这一定程度上决定了它们的生物活性(见空气污染颗粒:它们是什么?)。对于细颗粒,既要特别关注多环芳烃和醌类,也要关注金属组分。即便知道了颗粒的复杂组分,目前仍难以建立起单独颗粒组分与健康效应之间精确的因果关系。有研究表明,超细颗粒比大颗粒具有更高的生物活性。事实上,尽管超细颗粒仅占颗粒物的一小部分质量,但对于给定的体积,其数量更多,具备的反应面积更大。
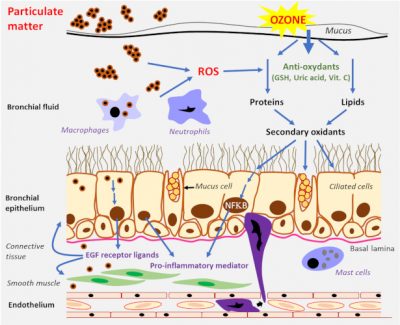
颗粒的主要作用机理为氧化应激[9],及其导致的炎症反应(图6)。氧化应激是一类由活性氧物质 (ROS) 及具有反应活性的氧化和氮氧化物质对细胞组分的攻击行为。最常见的三种活性氧物质包括超氧阴离子 (×O2) 、过氧化氢 (H2O2) 和羟基自由基 (×HO) 。活性氧物质的生成被认为是由细颗粒和超细颗粒诱发适应性反应或毒性事件的关键因素。在体内,活性氧物质等氧化物质和抗氧化防御机制之间始终维持着平衡。当防御机制处于下风时,就会出现炎症反应,并最终导致细胞坏死或凋亡(程序性细胞死亡)。在心血管中,动脉粥样硬化是血管壁的炎症过程,会导致动脉粥样斑块的形成和动脉损伤,是心肌梗死和脑中风的机制之一 。
如前所述,颗粒的组分是其毒性的决定因素之一。例如,过渡金属[10](如铁、铜、钒)可导致高反应活性的羟基自由基的生成。有机化合物(如醌类和多环芳烃)会造成巨噬细胞和支气管上皮细胞中生成活性氧物质。当颗粒与生物粒子或分子(如细菌或过敏原)相结合时,还会产生“特洛伊木马”效应。
3. 颗粒物的健康效应
目前已有诸多研究关注颗粒物的健康效应,难以一一赘述。这些研究大多涉及几十甚至几十万个个体。
3.1 死亡率
死亡率是研究最多的。各国的死亡率数据均易获得,而且死亡率对于潜在的环境健康效应而言,是一个很好的“指标”。所有的死因,无论是“自然死亡”还是“非自然死亡”,都被用来研究颗粒物暴露的关联性。
短期研究已表明,与污染爆发期相关的死亡数呈上升趋势[11] [12] [13] [14]。其中对PM10和PM2.5的研究最多。1987年至1994年间,针对北美地区90个主要城市开展的公民发病率、死亡率和空气污染的研究 (NMMAPS) 表明,PM10与死亡率之间存在微弱但一致的关系。在欧洲,对于PM10,PPHEA和APHEA2(欧洲的空气污染和健康效应方法)的研究得出了相同的结论。APHENA研究结合了北美和欧洲的研究结果,证实了研究方法和结果的可靠性。针对超细颗粒 (PM0.1)的健康效应研究仍较少,但也在印证这一趋势。
所有的队列研究也表明,自20世纪90年代以来,颗粒物暴露(特别是PM2.5)引起了长期死亡率的上升[6] [15]。在诸多死亡原因中,心血管疾病和心肺病因占主导地位,例如包括了22个队列研究,300000多名个体的欧洲ESCAPE研究(欧洲空气污染效应的队列研究)[16] [17]。另一项研究依据整个法国大都市的测定污染物浓度,考察了12年间主要大气污染物对死亡率的影响[18],证实了污染与长期死亡率之间的联系。该研究发现,即使浓度较低,颗粒物(PM10和PM2.5)也是造成死亡的主要原因,超过了氮氧化物和臭氧的影响。
许多研究还表明,颗粒物暴露减少可降低死亡率。特别值得关注是,长期以来人们一直认为只有急性污染期加剧才会增加健康风险。但现在表明,长期效应真实存在,并可能比短期效应更重要,这对减排措施和健康标准的制定具有重要意义。所有研究都表明,对于健康人群,颗粒物与死亡率存在联系。这一点一度是专家争论的焦点,尽管部分专家认为只有“脆弱”人群存在风险,但如今已达成共识。尽管如此,一些人群仍被视为存在更高风险,如糖尿病患者、有心肌梗死病史的患者、老年人和社会经济地位低的人。
最近由法国卫生组织进行的一项定量健康影响评估 (EQIS) 确立了接触PM2.5与死亡率[19]之间的关系(见图7)。这项研究估计,每年有48 000人死于PM2.5污染,相当于法国死亡率的9%。更准确地说,“如果法国各地由人为活动造成的PM2.5污染与污染程度最低的农村一样的话”,每年将有48000人免于死亡。这是模型估算的结果,也应被视作颗粒物污染对死亡率影响的估计值。在这种情况下,30岁的人将平均增加9个月的预期寿命。在巴黎,预期寿命的增加甚至可能超过两年。
这些结果与欧洲和国际评估是一致的。例如,欧洲环境署在2018年[20]的报告中估计,法国每年有35800人[21]因暴露于PM2.5而过早死亡,这一数字远高于氮氧化物和臭氧的影响。整个欧盟(28个国家)每年有391000人因暴露于PM2.5而过早死亡。世界卫生组织估计,全球每年约有700万人死于细微颗粒污染[22]。
总之,所有短期和长期的研究都表明颗粒物接触与死亡率之间存在显著的因果关系。
3.2 肺部疾病
由于颗粒的肺穿透性,可凭直觉预期其会对肺部产生影响。针对该问题的研究数量相当可观[6],主要包括PM10和PM2.5,对PM0.1的研究相对少,但研究结果具有相似性。
尤其是对幼儿的关注,因为他们的肺部和免疫系统仍未发育完全;此外,儿童每分钟的呼吸频率比成人高,且经常参与户外活动;并且,对于成人的肺部情况,幼儿的肺部情况是很好的预后因子。尽管结果不一且存在解释偏差,大多数短期研究表明,PM2.5暴露与肺部疾病和哮喘疾病的发生之间存在关联。人们还意识到,哮喘儿童对颗粒的效应要比健康儿童更敏感。长期研究证实了细颗粒与肺功能、肺发育和呼吸道症状之间的关联。
研究表明,空气质量的改善可减少儿童入院和呼吸系统疾病的频率。针对成年人开展的研究较少,但所有研究都表明,肺部效应的发生与颗粒暴露有关,特别是慢性阻塞性支气管炎的发展。
目前科学界一致认为,肺癌的发生与空气污染(特别是细颗粒)有关。2013年,空气污染和颗粒物的致癌性已被世界卫生组织国际癌症研究机构(IARC)认定 [23]。
3.3 心血管疾病
令人意想不到的是,空气污染和细颗粒物对心血管系统造成的风险看起来最大。所有的心脏病学会都经常警告污染会增加患心脏病的风险。大量短期研究表明,颗粒物暴露(PM10和PM2.5)与因心血管原因住院的频率之间存在显著关系。
长期研究尤其关注心力衰竭或心肌梗死的发生。另有研究关注心脏生理学方面更温和的变化,如心率变化或瞬时心肌缺血的发展,而这些变化往往能预示更严重的并发症。然而,由于这类研究实施困难,且难以获得一致性结果,目前还没有任何明确的结论。但所有研究发现都显而易见趋同,即颗粒物对心血管系统有害。
如前所述,颗粒物的主要毒性作用机制之一为炎症反应,这很可能会导致血管收缩,并发展成高血压。但是,有关高血压与颗粒物之间联系的研究结果大多并不显著,且有时相互矛盾,因而没有“明确”、一致的研究结论。
对于超细颗粒物,即便大多数专家认为PM0.1暴露与心血管效应之间存在关联,但目前研究尚少,难以得出定论。
3.4 神经系统疾病
一些短期研究表明,在急性污染期之后,细颗粒与中风(特别是缺血性中风)的发生存在关联。然而,相关的长期研究还很少。
少数研究考察了神经退行性疾病和长期认知障碍的发生。我们知道炎症过程在阿尔茨海默病或帕金森病的发展中起重要作用。最初的研究是以生活在墨西哥污染环境中的野狗为动物模型开展的,在这些野狗中检测到了炎性的脑部损伤。虽然一些人类研究表明,颗粒暴露和神经退行性疾病之间存在类似关系,但得出明确结论还为时尚早。
3.5 生殖障碍,围产期障碍
2005年,世界卫生组织已指出空气污染会对妊娠过程和胎儿产生影响。一些研究已经表明,空气污染(特别是颗粒物)会导致早产、低出生体重、胎儿畸形和婴儿死亡的发生。但是,由于胎儿敏感性在妊娠期不同阶段的变化,这使得比较研究困难重重。此外,其它解释偏见,如社会经济地位等的影响,很难断定妊娠期胎儿暴露存在可能的长久效应。即使一系列的争论认为颗粒物会产生有害的影响,但目前仍不能得出明确结论。
3.6 生物标记物
许多短期研究试图建立特定血液参数(特别是炎症和凝血标志物)与细颗粒暴露之间的联系,如众所周知的CRP(c反应蛋白,炎症标志物)、白细胞数、红细胞数和血红蛋白、纤维蛋白原等。试图寻找可以指示颗粒物暴露程度的、易于测量的血液标记物这一想法很吸引人。虽然有些炎症标志物貌似与颗粒物暴露有关,但结果过于碎片化,且无法得出一致的结论。
总之,目前尚无任何颗粒物暴露的生物标记物被鉴定。未来,相关研究的开展和分析技术的进步无疑将推动这方面的进展。
4. 健康标准
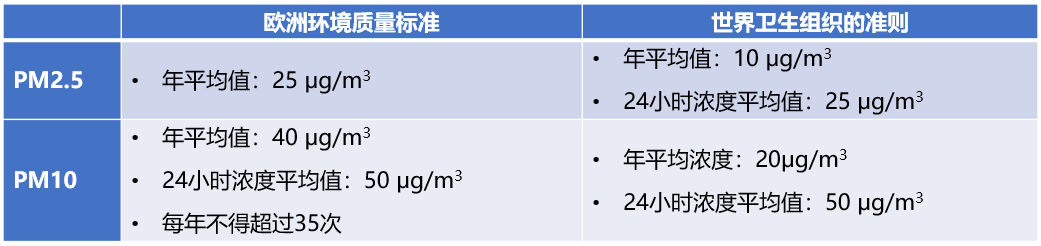
如本文开头所述,健康标准是基于估算和建模的结果,在世界各地都不统一[24]。
值得注意的是,世界卫生组织的指导值比欧洲标准更具保护性。法国的许多城市地区的空气质量经常超过欧洲标准。欧洲审计法院的一份相当严格的报告指出,包括法国在内的多个国家的减污染措施不足,未遵守健康标准[25]。
在法国,针对PM10的建议阈值和警报阈值分别为50 g/m3和80 g/m3[26] [27]。据估计,2017年,如果法国的所有城市都遵循世界卫生组织的PM2.5指导值,将会避免约17712人的死亡,相应的经济收益将达到530亿欧元[28]。
5. 社会经济成本
据欧盟参议院调查委员会估计,2015年,空气污染的经济和财政成本在700亿至1000亿欧元之间[29]。仅空气污染一项给法国卫生系统每年造成的损失就在10亿至20亿欧元之间,而为职业病额外支付的抚恤金高达10亿欧元。由疾病和过早死亡造成的社会福利损失难以精准确定,涵盖范围广泛,最高可达1000亿欧元。
2018年,欧盟参议院空气污染工作组声明,空气污染是一项健康危机,也是重大的社会经济问题。
大多数专家一致认为,实施重大污染减排措施的成本将远远低于污染造成的社会经济损失。前欧洲环境专员(2009-2014),雅奈兹·波托尼克 (Janez Potocnik) 是减少污染措施的坚定倡导者,他说“如果你认为经济比环境更重要,那就屏住呼吸数钱吧”[17]。
6. 要点
- 空气污染的健康效应毋庸置疑。
- 在各类空气污染物中,悬浮细颗粒物是引起健康效应的罪魁祸首。
- 长期以来,人们一直强调污染峰值期的危害。现在我们知道,长期污染可能比峰值污染水平更有害。
- 大量研究已经建立了颗粒物暴露与死亡率、肺部疾病和心血管疾病之间的因果关系。
- 尽管颗粒物对神经系统、妊娠期和生殖的影响还没有明确的结论,但一些研究已经指出颗粒物可能会引起不良效应。
- 目前对PM10和PM2.5的研究最多,而对PM0.1纳米颗粒的研究仍有待开展。
- 空气污染的社会经济成本巨大。
- 包括法国在内的诸多国家都未遵循现行的欧洲空气质量标准。
参考资料及说明
封面图片:[来源: ©Renée Grillot]
[1] Thompson JE (2018). Airborne particulate matter. Human exposure and health effects. Journal of Occupational and Environmental Medicine, 60, 5 : 392-416.
[2] www.who.int/fr/news-room/fact-sheets/detail/ambient-(outdoor)-air-quality-and-health .
[3] Ledrans M (2008). L’épidémiologie, un outil pour la veille et la décision en santé environnementale. Environnement, Risques & Santé, 7, 21-26. (in french)
[4] 混淆偏差:一种或多种不同于所研究的现象可以解释疾病。这项研究必须考虑到这种偏见。
[5] 因果关系:细颗粒物暴露对健康有许多影响。
[6] 相关性:两种现象并行发展,但不能确定其中一个导致另一个。
[7] Dab W. et al. (2001) Pollution atmosphérique et santé : corrélation ou causalité ? Le cas de la relation entre l’exposition aux particules et la mortalité cardio-pulmonaire. Journal of the Air & Waste Management Association, 51, 2013-218. (in french)
[8] Marano F. (2012). Mécanismes d’action des particules atmosphériques fines et ultrafines. Pollution atmosphérique (numéro spécial), 20-22. (in french)
[9] Baeza A (2007). Pollution atmosphérique et maladies respiratoires, un rôle central pour le stress oxydant. Médecine Sciences, 23, 497-501. (in french)
[10] https://en.wikipedia.org/wiki/Transition_metal
[11] Rückerl R. et al. (2011) Health effects of particulate air pollution: a review of epidemiological evidence. Inhalation Toxicology, 23 (10), 555-592.
[12] Kim K.-H. et al. (2015). A review on the human health impact of airborne particulate matter. Environment International, 74, 136-143.
[13] Kelly FJ et al. (2015). Air pollution and public health : emerging hazards and improved understanding of risk. Environ Geochem Health, 75, 631-649.
[14] Atkinson RW et al. (2014) Epidemiological time series studies of PM2.5 and daily mortality and hospital admissions : a systematic review and meta-analysis. Thorax, 69, 660-665.
[15] Burnett R et al. (2018) Global estimates of mortality associated with long-term exposure to outdoor fine particulate matter. Proceedings of the National Academy of Sciences of the USA, 115 (38), 9592-9597.
[16] Beelen R et al. (2014) Effects of long-term exposure to air pollution on natural-cause mortality : an analysis of 22 European cohorts within the multicentre ESCAPE project. Lancet, 383, 785-795.
[17] Mannucci PM et al. (2015) Effects on health of air pollution : a narrative review. Internal Emergency Medicine, 10(6), 657-662Encyclopédie de l’environnement 11/11 Généré le 27/02/2021
[18] Sanyal S et al. (2018) Long-term effect of outdoor air pollution on mortality and morbidity : a 12-year follow-up study for metropolitan France. International Journal of Environmental Research and Public Health, 15 (2487), 1-8
[19] Pascal M et al. (2016) Impacts de l’exposition chronique aux particules fines sur la mortalité en France continentale et analyse des gains en santé de plusieurs scénarios de réduction de la pollution atmosphérique. Saint-Maurice : Santé publique France ; 158 p. (in french)
[20] https://www.eea.europa.eu/publications/air-quality-in-europe-2018
[21] 过早死亡:在预期死亡年龄之前死亡,并考虑到有关国家的预期寿命。如果病因被消除就可以避免的死亡。
[22] https://www.who.int/fr/news-room/detail/02-05-2018-9-out-of-10-people-worldwide-breathe-polluted-air-but-more-countries-are-taking-action
[23] CIRC monography (2013) The carcinogenicity of outdoor air pollution. Lancet, 14, 1262-1263
[24] Annesi-Maesano I (2017) The air of Europe : where are we going ? European Respiratory Review, 26, 1-5
[25] Special Report No 23/2018: Air pollution: our health is still not sufficiently protected. European Court of Auditors. https://www.eca.europa.eu/Lists/ECADocuments/INSR18_23/INSR_AIR_QUALITY_E.pdf
[26] 信息和建议阈值:大气中污染物质的浓度水平,短期暴露在该浓度水平之上,会对需要立即获得充分信息的人群中特别敏感的人的健康构成威胁。
[27] 警报阈值:大气中污染物质的浓度水平,短期暴露在该水平之上会对一般民众的健康或环境退化构成风险,需要作出应急反应。
[28] www.amse-aixmarseille.fr/actualite/pollution-de-lair (in french)
[29] Sénat 2015 « Pollution de l’air : le coût de l’inaction ». Rapport n° 610 (2014-2015) by Mrs Leila AÏCHI, made on behalf of the EC economic and financial cost of air pollution, submitted on 8 juillet 2015. (in french)
环境百科全书由环境和能源百科全书协会出版 (www.a3e.fr),该协会与格勒诺布尔阿尔卑斯大学和格勒诺布尔INP有合同关系,并由法国科学院赞助。
引用这篇文章: DANEL Vincent (2024年3月9日), 空气颗粒物及其健康效应, 环境百科全书,咨询于 2025年4月2日 [在线ISSN 2555-0950]网址: https://www.encyclopedie-environnement.org/zh/sante-zh/airborne-particulate-health-effects/.
环境百科全书中的文章是根据知识共享BY-NC-SA许可条款提供的,该许可授权复制的条件是:引用来源,不作商业使用,共享相同的初始条件,并且在每次重复使用或分发时复制知识共享BY-NC-SA许可声明。