Zoonoses and environment
PDF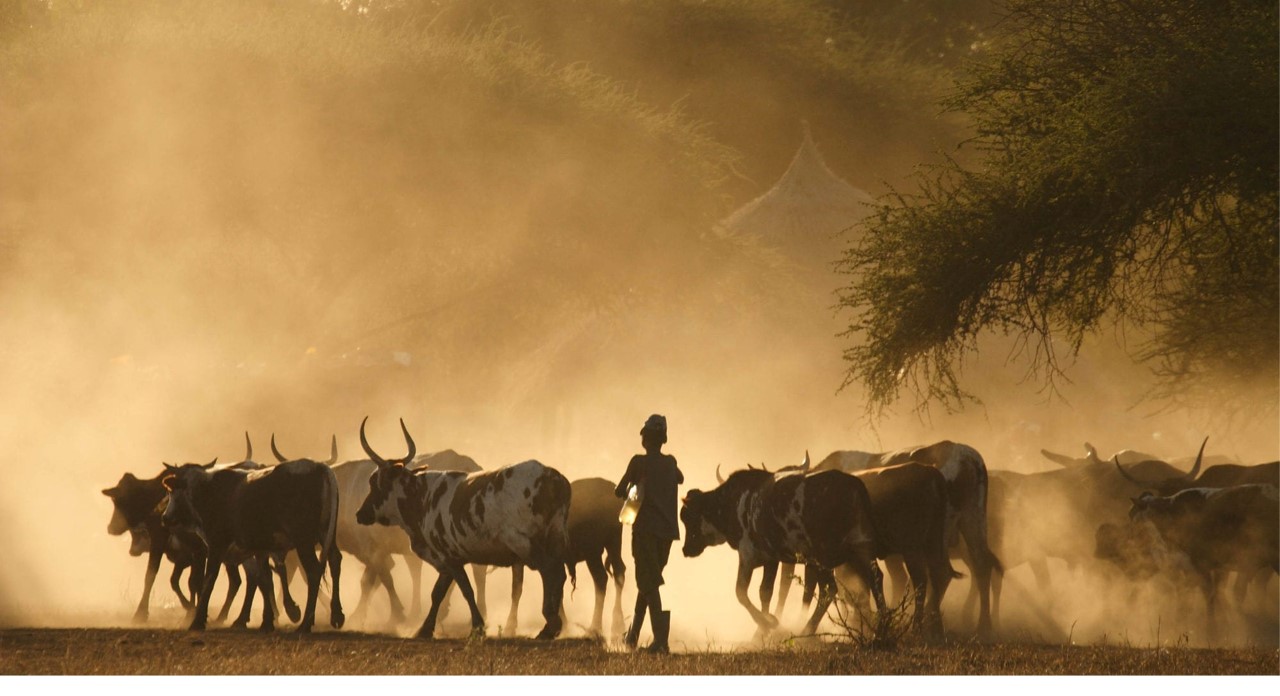
We still observe the appearance of Avian flu, coronavirus severe infections, Ebolavirus Disease, Lyme disease, monkey pox… but why do new diseases emerge regularly from animals, both wild and domestic? It has long been known that there are many infectious agents that can cause disease in both humans and animals. And that in some cases, infectious agents specific to animals can accidentally cross the species barrier to infect humans, causing a new and sometimes devastating disease in humans. This phenomenon, which is highly unpredictable and difficult to predict, nevertheless depends on numerous environmental, societal, and behavioural factors. What are the diseases shared by animals and humans? Where do the microbes responsible for them come from and how do they evolve? What are the transmission mechanisms from animals to humans? What are the risk factors and how can we prepare for the zoonotic risk? This article answers all these questions.

While there are infectious agents that are pathogenic only to humans, and others that are infectious only to one species or a limited number of animal species, there are many infectious agents that can cause disease in both humans and animals. The term ‘zoonosis’, a combination of the Greek words zoon, animal, and noson, disease, refers to these infectious diseases shared under natural conditions between humans and animals, whether wild, farmed or companion animals.
1.1. Prehistory: Human and nature, from prey to predator
At the dawn of humanity, hominids were fragile. They had many predators and survived by feeding mainly by eating carrion and gathering food. The invention of fire and the first stone tools helped humans to defend themselves: humans organized themselves socially, defended themselves against aggression and became predators in their turn. They adapted to the environments they encountered and mastered the art of hunting wild animals (Figure 2). Human evolution is thus punctuated by encounters between humans and animals, and the transmission of infectious micro-organisms from one species to another is permanent.

1.2. Modern history: Human is moving away from nature
With the age of industrialization, the advent of technology, rapid urbanization and modern lifestyles, the distance between man and nature has undeniably reduced the risk of contamination by an infectious agent from wildlife. For example, contact with bats and rats, vectors of many diseases, has been greatly reduced in modern times. On the other hand, some animals are seeing their habitat reduced or changed because of human activity or environmental changes (climate, land use, mobility, etc.), forcing them to leave their wild environment or modify their behavior, bringing them closer to humans. And more and more humans are coming into close contact with pets.
1.3. The importance of zoonoses
It is estimated that more than half of all human infectious diseases originate in animals. Zoonoses are responsible for more than two billion cases of disease in humans every year, with the occasional danger of direct human-to-human transmission and epidemic or even pandemic development of certain zoonoses. The frequencies are uneven: some zoonoses are very common, in many countries; others are present only in specific geographical areas; finally, some are exceptional, even if their epidemiological consequences can be significant (Ebola, SARS-CoV). The medical consequences of zoonoses in humans are highly variable: some are benign and easily curable (taeniasis, etc.), while others can be fatal (rabies, Ebolavirus disease, etc.). Finally, zoonoses have major consequences for the animals themselves: wild species can be threatened with extinction, ecosystems can be disrupted, and the economic consequences for livestock farming can be very significant, as in the case of avian influenza, for example.
Among the many zoonoses, those that are likely to evolve into human-to-human transmission are particularly dreaded (see Focus Zoonoses diversity). As the human population is immunologically naïve (with no specific acquired immunity to new pathogens) to the emergence of an infectious agent from the animal world, the health consequences can be disastrous, as recent history has shown in the case of influenza viruses, hemorrhagic fever viruses and coronaviruses.
2. Zoonoses: mechanisms of transmission
Zoonoses can be caused by different types of infectious agents: bacteria or rickettsia (obligate intracellular bacteria), viruses, prions, parasites, fungi. The notion of transmissibility is important: some diseases are common to animals and humans, but are not transmitted from one to the other, and are therefore not considered zoonotic diseases (e.g., tetanus). Most diseases that are transmitted from animals to humans are usually not transmitted (or very difficult) between humans. Only a few zoonotic diseases have had the ability to develop human-to-human transmission.
The emergence and spread of a zoonosis can thus be summarized in several stages:
- Contact between humans and animals carrying the infectious agent;
- Transmission of the microbe between animals and humans (sometimes with the intervention of an intermediate host or vector);
- The adaptation of the microbe from the animal world to the human host, followed or not by possible human-to-human transmission.
What is remarkable in this mechanism is the transgression of the species barrier, i.e., the passage from one species to another: the infectious agent must modulate or modify its mode of development – and therefore of survival – to adapt to this new species. Finally, it should be noted that all pandemics in the last century have originated in animals (See Viral pandemics of the modern era).
2.1. Zoonotic risk
The risk factors related to the transgression of the species barrier are of two types: sociological and environmental factors influencing the probability of contact between humans and animals, and biological factors related to the adaptation of the infectious agent to a new host:
- For most microbes, there is a strict specificity for a species susceptible to infection. This specificity is related to the penetration of the envelope (epidermis, mucous membranes), the recognition and penetration by the microbe of the target cells, and the escape of infective forms from the host.
- Contact with wild animals promotes the emergence of new infectious diseases. The opportunities for these contacts have generally decreased sharply with people development, but they have changed in nature: they are increasingly linked to tourism, deforestation, hunting and wildlife trafficking.
- Whether they are farmed or petted, domestic animals present a proven risk of zoonotic transmission. Multiplying the risk of contact with pathogens that are found in the wild, they can also act as intermediate vectors. Worldwide, it is estimated that there are more than one and a half billion pets. There are hundreds of billions of farm animals.
2.2. Direct and indirect transmission
There are two main mechanisms of transmission of a pathogen during animal-human contact:
- Direct transmission. The infectious agent is transmitted from an infected animal to a susceptible host (human or intermediate host) through contact with a biological excretion product (saliva, blood, urine or feces). Contact can be transcutaneous or on skin lesions, mucous membrane (licking), airborne (airborne droplets emitted by an infected animal), gastrointestinal (infected food), or blood (bite) (Figure 3).

- Indirect transmission. The infectious agent is transmitted via a vector. Vectors can be of several types:

Figure 4. Aedes aegyptii in the blood meal phase. Some mosquitoes are vectors of viral or parasitic diseases (dengue, chikungunya, Japanese encephalitis, yellow fever, malaria, etc.). [Source: photo (c) James Gathany, Public domain, via Wikimedia Commons]
(i) Inert vectors, such as contaminated materials (sharp objects, surfaces), insects infested on their sharp/stinging/sucking parts, but which do not enter the natural reproductive cycle of the microbe (e.g., the house fly, Musca domestica, known for its role as a mechanical vector in the spread of various infectious diseases such as shigellosis, salmonellosis, staphylococcal disease).
(ii) Active vectors (mosquitoes, flies, mites, fleas, ticks, rodents, or other vertebrates) necessary for the natural cycle of the pathogen (multiplication in the vector and transmission) (Figure 4). There are many examples: the plague bacillus and flea, Borrelia and ticks, Lassa fever virus and multi-udder rats, arboviruses and Culicidae mosquitoes or mites. These vector-borne diseases have characteristics related to their vector and their transmission cycle.

- Transmission via consumer products: it occurs during consumption (undercooked infested meat or flesh, raw milk), when consuming products contaminated with the feces of an infected animal (fruits, vegetables, cereals), or during handling of infected animal products (butchering, transport, preparation) (Figure 5).
2.3. The emergence of zoonoses
Zoonotic outbreaks are rare events, difficult to predict in time and space, but their probability increases as soon as the risk over the long term is considered. Certain factors, biological, social, environmental, behavioral, increase the probability.
2.3.1. Risk factors for emergence
The emergence and spread of a zoonosis result from events involving multiple factors:
- Factors related to the probability of an encounter between animals and humans;
- Ability of the pathogen to mutate biologically for transgression of the species barrier and adaptation to a new host;
- Environmental and behavioral conditions favorable to transmission processes and possible vectors.
The transgression of the species barrier is the main mechanism for the emergence of a zoonosis. Two essential events are necessary for this mechanism:
- The meeting of two species and the exchange of microbes: this is the overflow of species, better known in the literature under the English term ” Spillover “.
- The survival of the microbe in the species that receives it: if the species does not multiply it or rejects it, the exchange fails, and the episode ends with the disappearance of the infected individual. If the recipient species multiplies the microbe, then there is a transgression of the species barrier and the possible emergence of a zoonosis.

- The genetic plasticity of the pathogen (mutation, recombination, reassortment) which, for some, can be high and allows them to adapt to a new host.
- Host specificity: Some pathogens have low host specificity and can infect related taxa species.
- The proliferation of hosts living in sympatry (e.g., rodents, mosquitoes) can be a determining factor in promoting contact with vulnerable hosts.
- Factors related to the natural environment (climate, natural disasters, etc.) or of anthropogenic origin (population density, human and animal mobility, urbanization, deforestation, fragmentation of natural areas, agricultural and livestock practices, etc.) can promote the emergence, extension and endemic of a zoonosis (See Climate change: what effects on our health?).
2.3.2. Examples of risk factors for emergence
2.3.2.1. Behavioral factors
- The emergence of Lyme disease in humans is thought to be due to increased contact with species naturally infected with the bacteria responsible for the disease. In the USA, deer and rodents, natural hosts of the tick-borne Borrelia, have begun to proliferate because of hunting regulations. Subsequently, the development of housing outside urban areas, more in contact with forest edges, probably contributed to the emergence of the disease, then to its spread in the northeastern United States and Canada.

Figure 7. Chiroptera (bats) are recognized as hosts, reservoirs and vectors of many viruses that are pathogenic to humans. [Source: authors’ montage from two photos; background: Cave with bats, El Maviri Sinaloa, Mexico © Tomas Castelazo, www.tomascastelazo.com / Wikimedia Commons – in the foreground Rousettus aegyptiacus, Original photo: אורן פלס Oren Peles Derivative work: User:MathKnight, CC BY 2.5 License, via Wikimedia Commons] - Ebola fevers. In Central Africa, some species of bats could be chronically infected by the Ebola virus and be its natural reservoir (Figure 7). Wild animals susceptible to infection by the virus (primates, wild ungulates) can become infected through contact with this reservoir or its infected biological products. Human contamination could be linked to exposure in the forest (hunting, butchering of wild animals). Human-to-human spread involves other factors, related to dietary habits (bushmeat consumption) and social behaviors (ritual or religious practices, especially during funeral ceremonies).
- Monkeypox. Many species of primates and rodents have been found to carry the virus. The disease is transmissible to humans and has symptoms like those of smallpox, but with less severity (See focus From smallpox to Mpox: a renewed threat). In May 2022, cases of monkeypox were reported to WHO by non-endemic states for the virus and followed more than 62,000 cases in 105 countries and territories, with 23 deaths. Fortunately, the historic smallpox vaccine, many doses of which are still being preserved, proved effective against monkeypox, and brought this pandemic to a halt.
- Cryptosporidiosis is a cosmopolitan disease that manifests itself as severe diarrhea in animals (cattle, birds) and humans. Transmission occurs mainly through contact with the environment contaminated by the excrement of contaminated animals, via the environment (rivers, pastures, gardens) or through direct contact with animals via the fecal-oral route. Between 2001 and 2010, Cryptosporidiosis was the leading cause of recreational water illnesses in the United States.
- Alveolar echinococcosis is a serious parasitic disease caused by the development of larvae of the tapeworm Echinococcus multilocularis in humans. The parasite is present in dogs, foxes, and other wild carnivores. Humans can contract the disease through food contamination by accidentally ingesting eggs of the parasite present in the environment (e.g., on wild berries). Alveolar echinococcosis is characterized by an asymptomatic incubation period of 5 to 15 years and the slow development of a tumor lesion localized in the liver, accompanied by weight loss, abdominal pain, generalized malaise and liver failure. If left untreated, alveolar echinococcosis is fatal.
- Verno-summer meningoencephalitis (MVE). The seasons can influence the transmission of certain zoonotic diseases. For example, outdoor activities such as camping, and hiking increase the risk of contact with ticks. EVD is a disease caused by a Flavivirus transmitted by the bite of an infected rodent tick, abundant in summer.
2.3.2.2. Social vulnerability and poverty
Zoonotic diseases are often linked to poverty and the resulting vulnerabilities: precarious living conditions, fragile health systems, limited access to safe drinking water and sanitation, close contact with farm animals.
- Chagas disease, or American trypanosomiasis. It is estimated that 6 to 7 million people worldwide are infected with Trypanosoma cruzi, the parasite that causes the disease. It is transmitted mainly through vectors, through contact with the stool or urine of triatomine bugs infected with T. cruzi, as well as orally (foodborne transmission), through blood and blood products, or from mother to child (congenital transmission). Contact with triatomines is strongly linked to the socio-economic vulnerability of populations and the hygienic conditions of habitats. The disease is mainly found in Latin America.
- Leptospirosis. A disease transmitted by bacteria of the genus Leptospira, which are usually found in the urine of rodents. People living in areas of precarious or unhealthy housing (poor sanitation, risk of flooding, environment in contact with rodents) are more exposed to this disease.
- Rift Valley Fever. This livestock disease in tropical areas is caused by a virus transmitted by mosquitoes. Farmers can become infected through contact with the blood or tissues of infected animals. Populations living in rural areas and who depend on agriculture or livestock farming are particularly at risk.
- Leishmaniasis, caused by protozoan parasites belonging to more than twenty species of Leishmania, is transmitted by the bites of sandflies. Disadvantaged populations living in enzootic regions with precarious housing conditions are at increased risk of exposure to bites from infected sandflies. It is estimated that 700,000 to 1 million new cases are added each year.
2.3.2.3. Promiscuity with Pets
- Toxocariasis and pets. Human toxocariasis (fever, abdominal pain, respiratory syndrome) is a parasitic infection caused by the larvae of roundworms (Toxocara canis or Toxocara cati) that occurs after accidental ingestion of the eggs of these intestinal parasites of dogs and cats. Eggs are abundant in the feces of infected cats or dogs (200,000 eggs per day per parasitic worm), and transmission in humans is usually through objects, surfaces, soiled food, or water contaminated with eggs. Flies can also spread eggs on surfaces or food.
- Cystic echinococcosis of shepherds. Cystic echinococcosis is a cosmopolitan zoonosis caused by an infection of the larval stage of Echinococcus granulosus (tapeworm) that infects dogs. The mode of transmission to humans is the accidental consumption of water or food contaminated with the feces of infected dogs.
2.3.2.4. Climatic and environmental factors
- Vector-borne diseases. Diseases transmitted by vectors, in particular mosquitoes (such as malaria, or many arboviruses such as dengue, chikungunya, West Nile virus encephalitis, Japanese encephalitis, Zika virus disease, etc.) or ticks (such as Lyme disease or tick-borne encephalitis) are dependent on the abundance and activity of these vectors. The risk of transmission of vector-borne diseases is increased when climatic conditions are favorable to vectors.

Figure 8. Migratory birds in training can be vectors and reservoirs of many viral zoonoses [Source: photo license CC0, via PxHere] - Seasonal animal behavior. Some zoonotic diseases have seasonal peaks due to animal behavior linked to climatic factors. For example, the risk of leptospirosis is increased during the rainy season, when infected rodents leave flooded areas or floods can spread bacteria. Seasonal migrations of animals can influence the spread of zoonoses: migratory birds (Figure 8) can carry viruses over long distances; Rift Valley fever virus is carried by transhumant cattle in the Sahel countries during the dry season in search of pasture and water.
- Seasonal agricultural practices. In areas where agriculture is seasonal, harvest periods may be associated with an increased risk of zoonotic diseases related to the use of livestock in contact with wild animals. For example, Junín’s hemorrhagic fever in Argentina, whose epidemic manifestations correspond to the maize harvest and contact with rodents in fields infected with the virus; the seasonality of yellow fever in Brazil, the incidence of which increases at the time of harvest or planting of rice and soybeans.
- Nipah virus and El Niño. Due to exceptional drought, deforestation and an abnormally high temperature caused by the El Niño phenomenon, huge forest fires in Sumatra have forced the migration of bats from Sumatra to the Malay Peninsula. Infected bats introduced an unknown virus into the agricultural region of Nipah, where it was first identified. Farm animals have been infected by fruit soiled by bats in search of food resources.
- Borreliosis and the Sahelization of Forest-Savanna Ecosystems in West Africa. African borreliosis, or tick-borne relapsing fever, is a serious disease with meningoencephalitis complications. Small wild mammals serve as reservoirs for the responsible borrelia, and humans can be infected by the bite of the vector tick. Climatic variations in the sub-Sahelian region have caused an extension of the geographical distribution of the tick. Tick-borne African borreliosis now has a high incidence in the Sudanian savanna zone (south of its historical enzootic zone) where it was previously absent.
2.1.2.5. Dietary risk
- Meat parasites. Intestinal or muscular sarcocystosis is mainly due to the ingestion of cysts of Sarcocystis hominis (protozoan parasite of bovids) or Sarcocystis suihominis (protozoan parasite of pigs) contained in meat for consumption. Trichinellosis (T. britovi, T. spiralis, etc.) is caused by the consumption of raw or undercooked meat prepared from infected animals, such as pork, wild boar and wild bear. Tapeworm is contracted by ingesting cysticerci contained in undercooked pork (Taenia solium) or beef (T. saginata). Ingestion of T. solium eggs by human-to-human oral-fecal transmission can lead to cysticercosis.
- Salmonellosis is a zoonotic disease caused by bacteria that live in the intestinal tract of many mammals and birds. Each year, Salmonella causes hundreds of millions of infections worldwide, with more than 150,000 deaths. 85% of infections are related to food. The risk is linked to contact with animals or products contaminated by their droppings, and the eating habits of consuming raw or undercooked products.
- Brucellosis is an infectious disease caused by a variety of bacteria of the genus Brucella that mainly infect sheep, cattle, pigs, goats, and dogs. Humans can become infected through contact with infected animals, by drinking or consuming animal products contaminated with the bacteria (mainly raw milk or unpasteurized dairy products), or by inhaling contaminated particles. Human-to-human transmission is rare.

Figure 9. Fillet of Pacific salmon (Oncorhynchus keta) with a live parasitic nematode (Anisakis sp.). [Source: photo © Togabi, CC0 license, via Wikimedia Commons] - Anisakiasis and seafood. Anisakiasis is a disease caused by nematode worms (e.g., Anisakis, Pseudoterranova spp.) that infect fish (Figure 9) and marine mammals, and occasionally other marine organisms such as squid and octopus. Infection occurs through the consumption of fish or seafood infected with Anisakis larvae, eaten raw, undercooked, or marinated (e.g., sushi or ceviche). Anisakiasis is manifested by severe abdominal pain, nausea, vomiting and diarrhea, with in some cases allergic reactions.
3. Public health: analysis and prevention of zoonotic risk
3.1. The systems approach to health
For a long time, the study of human diseases was limited to the search for therapeutic solutions and care, far from a “public health” vision. Since the beginning of the twentieth century, a much broader approach has developed in the wake of scientific advances in microbiology, epidemiology, and statistics. The deciphering of a state of health no longer calls only on the characteristics of the pathogen and the individual, but also on those of the population to which it belongs and the characteristics of its environment, natural, social and cultural. These parameters concern in particular the relationships between individuals (proximity, contacts, behavior’s, etc.), relations with other living beings in the animal or plant world, and exposure to their environments (“One Health“).
The systems approach to health thus considers a health phenomenon as a complex system made up of active “agents” that act and interact according to their individual and collective characteristics, and the environments to which they are exposed (Figure 10).
The systemic approach makes it possible to approach the study of zoonoses by considering all the parameters necessary to understand the phenomenon studied.

3.2. Risk: a combination of hazards, exposure to hazards, and vulnerabilities
In a “public health” approach, this systemic framework can be approached from a “risk” perspective, separating what is the responsibility of the threat and what is the responsibility of vulnerability (i.e., the ability to be affected by a threat):
- The threat (or “hazard”) can be the presence of a pathogen, a vector, a reservoir, pollutants, harmful substances, noise, high-risk industrial presence, etc.
- The susceptibility of the individual (essentially due to individual, genetic and biological characteristics – such as immune status, or age) is strongly linked to the pathology.
- The “passive” vulnerability of the individual, which does not necessarily depend on the pathology, but which can influence the individual’s exposure to the threat or his or her protection from the pathology.
- “Active” vulnerability, which includes all factors that are likely to increase the individual’s direct exposure to the threat.
3.3. Zoonoses and Public Health
This pragmatic approach is particularly suitable for the study of zoonotic risk. It differentiates:
- Natural biological threats, which are often subject to a high degree of random variability in time and space (certain events with a low or even very low probability must sometimes be taken into account, such as the emergence of a pathogenic agent from the animal kingdom, which is often impossible to predict or control);
- Vulnerability, which is generally much more stable at the level of human populations or infrastructures, and which allows for better public health action.
This is called preparation rather than forecasting, and even less so prediction. This approach also enables crisis situations to be dealt with rationally:
- On the one hand, by preventively targeting the most important or most fragile elements of the system, in terms of vulnerability (the issues at stake, such as the healthcare system);
- Secondly, by optimizing management and actions to urgently reduce the threat (elimination of vectors, isolation, slaughter of infected animals, etc.) or the susceptibility and exposure of the population (vaccinations, hygiene, protection, quarantines, confinement, etc.).
4. Messages to remember
- Zoonoses, diseases of animal origin, remain a major threat to human health: more than two-thirds of the infectious diseases currently emerging come from wild or domestic animals.
- It is impossible to eradicate pathogens that are kept in the environment by wildlife. Reducing the susceptibility of wildlife or farm animals to a particular pathogen through vaccination is sometimes possible, but always with relatively low effectiveness.
- In the case of diseases transmitted by insects (mosquitoes, ticks, bugs, etc.), attempts can be made to eradicate the pathogen by vector control, but this is often a difficult battle.
- Preparing for the risk of zoonoses emerging and spreading is essential, especially when the emergence may be followed by human-to-human spread, leading to epidemic or pandemic events. Risk preparedness essentially concerns the vulnerability of human and animal (farm and domestic) populations: hygiene practices, behavior, eating habits, exposure to vectors (mosquito nets), farming practices, farm biosecurity.
- To avoid the risk of an epidemic or even a pandemic when direct human-to-human transmission occurs after transgressing the species barrier from animal to human, preparedness involves setting up surveillance and early warning systems to limit the spread of the infectious agent before it gets out of control.
- Preparing for the risk of an epidemic also means drawing up crisis management plans, including preparing the healthcare system to avoid bottlenecks and shortages of equipment or medicines, as well as measures to reduce people’s exposure to the pathogen if necessary.
Notes and references
Cover image. A boy returns home with his family herd at dusk in the village of Lhate, Chokwe, Mozambique, where several zoonosis are circulating, including the Rift Valley Fever Virus among others. [Photo source: © ILRI/Stevie Mann, CC BY-NC-ND 2.0 Deed license].
The Encyclopedia of the Environment by the Association des Encyclopédies de l'Environnement et de l'Énergie (www.a3e.fr), contractually linked to the University of Grenoble Alpes and Grenoble INP, and sponsored by the French Academy of Sciences.
To cite this article: GONZALEZ Jean-Paul, SOURIS Marc (January 5, 2025), Zoonoses and environment, Encyclopedia of the Environment, Accessed January 29, 2025 [online ISSN 2555-0950] url : https://www.encyclopedie-environnement.org/en/health/zoonoses-and-environment/.
The articles in the Encyclopedia of the Environment are made available under the terms of the Creative Commons BY-NC-SA license, which authorizes reproduction subject to: citing the source, not making commercial use of them, sharing identical initial conditions, reproducing at each reuse or distribution the mention of this Creative Commons BY-NC-SA license.