气候变化:对我们的健康有什么影响?

2030-2050年,气候变化预计每年将导致近30万人死亡,增加儿童营养不良与失调、虫媒传播疾病、腹泻和热应激日益增多。气候变化对健康的潜在影响是多重的。除此之外,农业产量下降、洪水、海平面上升等会造成人类生活、环境的深刻变化,往往会导致人口迁移,预计到2050年,将会有近2.5亿“气候难民”。人们应该还记得2003年欧洲夏季高温导致的超高死亡率,仅8月份就有7万人死亡。气候对传染病的影响更为复杂,但昆虫学家们相信全球炎热且潮湿地区的扩张将使携带病毒的昆虫数量增加10倍。最后,气候变化将对经济产生的影响不言而喻:到2030年,估计对健康造成的直接损失将在20至40亿美元之间。
1. 令人震惊的事实
过去的130年,全球气温上升了约0.85℃,主要是温室气体浓度升高引起的。近25年来,气候变暖的速度加快,平均每10年上升超过0.18℃[1]。气候变化下,海平面上升,冰川融化,降水分布也在变化。此外,还有其他更难观测的复杂气候变化,比如愈演愈烈的极端天气事件(干旱、洪水、热浪)(参见热带气旋:影响和风险)。气候变化产生的有利影响少之又少(例如降低温带地区冬季死亡率),往往是对公众健康带来威胁。例如,气候变化导致大多数农作物产量下降。政府间气候变化专门委员会(IPCC)在第五次评估报告中指出,在极端天气事件(重大火灾、风暴、洪水)之后,食品和谷物价格通常会迅速上涨[2]。
气候变化及其后果已经且仍将对最贫穷人口造成巨大影响,他们购买食物更加困难。英国杂志《柳叶刀》于2009年发表的一篇报告将气候变化确定为21世纪全球所面临的最大公共健康威胁[3]。2018年11月29日星期四,《柳叶刀》杂志发布了《柳叶刀倒计时》报告的第二版,专门探讨了气候变化对健康的影响。此报告是五大洲的27个学术机构、联合国各组织间和政府机构间的合作结果,揭示了因为气候变化全球人类在当前和未来所面临的“不可接受的”风险。
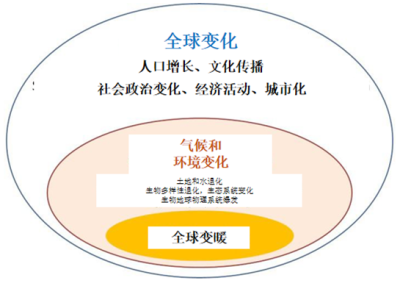
总而言之,如今气候变化带来的影响已显而易见,而且预测未来它会对人类健康产生难以接受的潜在灾难性风险。此外,全球变暖引发的人类健康风险又是叠加在全球化(人口变化、社会变化、经济活动)引起的人类健康风险之上的[4]。
2. 对人类健康有什么影响?
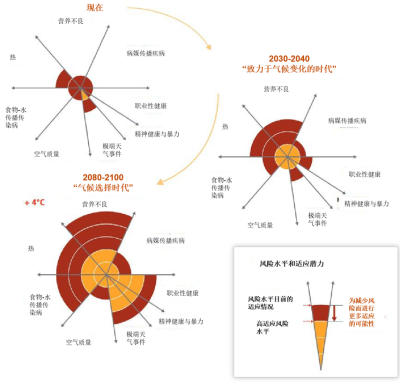
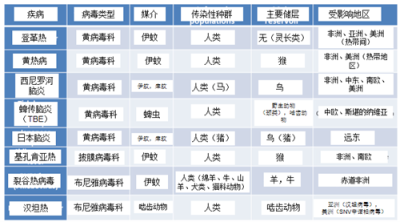
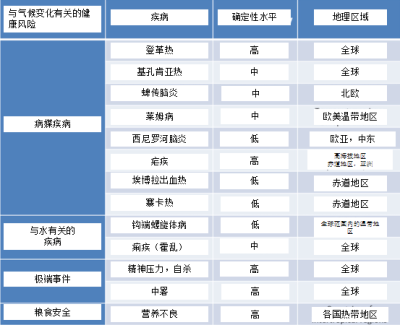
图1总结了气候变化对人类健康的影响。总的来说,可以分为直接和间接两种影响:
(a) 直接影响:营养失调与不良(可能是最重要的)、极端事件(如热浪)造成的死亡率和发病率升高、传染病(病媒传播和食物-水媒传染病)导致的死亡率和发病率升高。
(b)间接健康影响:可利用的水资源、可获得的食物、海平面上升等。
许多其他疾病也与气候变化有关:
(a)极端事件及其可能导致的迁徙现象对气候难民造成的创伤后精神压力;
(b) 空气污染(如臭氧含量随温度的升高而增加)相关的呼吸系统疾病。气温上升也会导致过敏发病率上升。在气候变化下的评估更为复杂。
此章节中,我们先阐述那些直接且无可争议的影响(如热浪),然后讨论与气候以外许多因素(尤其是地缘政治和人口)相关的更为复杂的主题(如营养不良)(图2)。
2.1. 致命的热浪
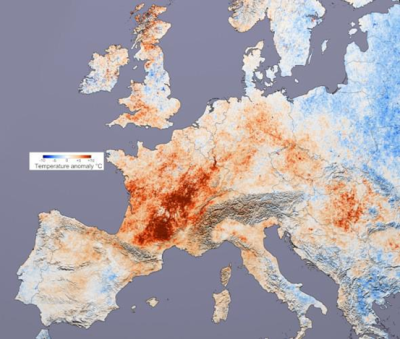
Temperature anomaly,气温异常。
2003年8月上半月创下了多项16世纪以来的高温历史纪录 [5]。此次热浪伴随着异常炎热、干燥的春季而来,一些地方4月末气温已达到30摄氏度。这次酷暑再加上创纪录的干旱让人回想起1947年夏天欧洲的热浪和1976年的干旱(图3)。在某些国家,如法国或葡萄牙,极端气候对生态系统、农作物产量(法国减少了20%)、人口和基础设施造成了重大影响,甚至引发政治危机。目前,不同数据来源(Inserm,INSEE,INEIN,France)一致显示法国约有15000人因热浪而死亡,死亡率增加了55%!死亡人数过多主要集中在老年人中,75岁以上老年人受影响最大。同一年龄段,女性比男性受到的影响更严重。主要症状是肌肉痉挛、高温引起的器官衰竭、中暑死亡(心血管失代偿)。
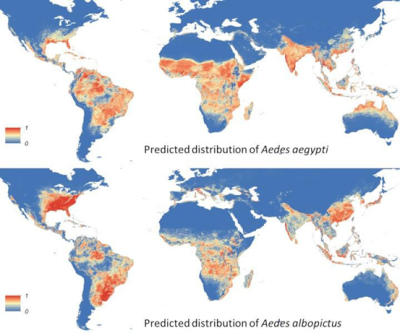
Predicted distribution of Aedes aegypti, Predicted distribution of Aedes albopictus.
埃及伊蚊的预测分布,白纹伊蚊的预测分布。
2003年欧洲的高温热浪仍将作为先前和后续同类事件的参考点。此后,世界各地的其它高温事件都被记录下来,特别是2012年夏天美国的高温事件(图4),热浪之后,经过温和多雨的冬天, 西尼罗河脑炎(病毒性脑炎-西尼罗河病毒)病例增加[7](见表1)。最近的一项研究得出以下结论,世界上近三分之一的人有可能受到致命热浪的威胁,如果温室气体排放量继续以目前的速度增长,到本世纪末,这一比例可能上升到四分之三[8]。
2.2. 病媒传染病呈上升趋势
2.2.1. 总体数据
虫媒传染病的传播是由以下几个因素决定的:(i)冬季气温升高会延长昆虫的活跃期(繁殖增加),从而改变蚊媒疾病和蜱传疾病的流行病学特征(由于缺乏滞育阶段而持续传播),滞育在生物体发育过程中由遗传决定的,在此期间代谢活动的强度降低)。(ii)为了抗旱,建造蓄水池储水,导致蚊子滋生。(iii)降雨为蚊虫的孳生创造了繁殖场所。
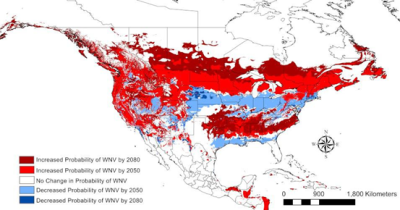
Increased Probability of WNV by 2080, Increased Probability of WNV by 2050, No change in Probability of WNV by 2050, Decreased Probability of WNV by 2050, Decreased Probability of WNV by 2080.
截止2080年WNV传播概率增加的区域增加,截止2050年WNV传播概率增加的区域增加,截止2050年WNV传播概率不变的区域无变化,截止2050年WNV传播概率降低的区域,截止2080年WNV传播概率降低的区域。
因此,蚊媒病毒[9]-虫媒病毒(节肢动物传播的病毒)的地理分布应该会扩大。这种情况会导致黄热病、登革热及出血并发症的病例数量总体增加。一些虫媒病毒是由伊蚊属蚊子(250种携带多种病毒)传播的,它们对气候变化非常敏感。白纹伊蚊是基孔肯雅病毒、登革热和寨卡病毒等病毒性疾病的传播媒介,在世界范围呈扩散趋势,它起源于亚洲,飘洋过海,成为当今地球上最具侵入性的媒介之一[10](图5)。白纹伊蚊已在包括法国在内的约80个国家中被发现,这种双翅目昆虫适应性很高,通过卵进行传播,雌性通常在不流动的积水中产卵。
此外,硬蜱属的蜱虫在温暖环境下活力最强。因此,随着全球变暖,预计这些昆虫传播导致的脑炎发生频率将增加(见表1)。
2.2.2. 几个病媒疾病的实例
第一个虫媒病毒的例子是登革热,受全球变暖的影响,其发病率增加[11]。该病毒由埃及伊蚊和白纹伊蚊传播,主要集中在美洲、非洲和亚洲的赤道地区。世界和欧洲范围内病例数量日趋增多[12]。根据世界卫生组织估计,全球约有25亿人面临感染登革热的风险,每年会有5000万人罹患登革热以及50万例出血性登革热病例,其中大部分患病儿童需要住院。专家估计,到21世纪80年代,可能还会有30亿人有罹患登革热的风险[13]。
西尼罗河病毒(WNV)由库蚊属蚊子携带,可传播给鸟类和哺乳动物,也包括人类。它于1999年出现在美国,并于2012年强势复苏,证明了气候变化在这个地区的作用(表1和图5)。自该病毒传入北美以来,已经感染了数百万美国人,78万人患病,超过1.6万人患上脑炎,1549人死亡[14]。
对于某些病毒性疾病,病例数量的增加是由于全球变暖以及与全球变化有关的现象导致的。例如,在拉丁美洲,森林砍伐和城市化已经改变了登革热的流行病学特征,它已从地方性动物病发展为城市流行病。登革热描述了一种独特的动物性疾病特征,它的发病率在动物中通常相当稳定,且在森林区传播;在人类中的发病率通常也相当稳定,在城市中传播[15]。 我们扪心自问,非洲愈演愈烈的埃博拉病毒(随着时间推移),以及最近拉丁美洲出现的寨卡病毒,是不是气候变化的后果之一[16]?
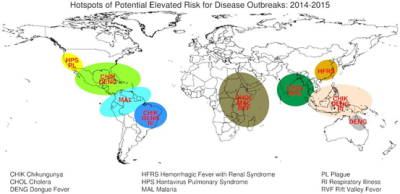
Hotspots of Pptential Elevated Risk for Disease Outbreaks:2014-2015.
疾病暴发风险升高的热点地区:2014-2015。
CHIK Chinkungunya,CHOL Cholera, DENG Dengue Fever, HFRS Hemorrhagic Fever with Renal Syndrome, HPS Hantavirus Pulmonary Syndrome, MAL Malaria, PL Plague, RI Respiratory Illness, RVF Rift Valley Fever.
CHIK基孔肯亚热,CHOL霍乱, DENG登革热, HFRS 流行性出血热, HPS 汉坦病毒肺综合征, MAL疟疾, PL瘟疫,RI 呼吸系疾病,呼吸器官疾病, RVF山谷热.
但还有其他伊蚊属蚊媒病毒的例子:
(i) 基孔肯雅病毒感染已在非洲和亚洲广泛传播(图6)。其病症为发热性关节疼痛,在意大利本地的传播有所增加。这种蚊媒疾病在法国也广泛存在。
(ii) 裂谷热病毒(RVFV)是牲畜罹患动物流行病的原因。人类和动物之间的接触感染增加了病例数量,并向北部扩展(沙特阿拉伯)(图6)。
冈比亚按蚊携带的疟疾病原体(间日疟原虫和恶性疟原虫),在肯尼亚已观察到疫情,特别是在海拔2000米以上、温度超过18°C以及降雨量每月超过15厘米[17]的区域。居住在高海拔地区的人群感染疟疾的机率较高,这取决于山区变暖的程度[18]。
2.3. 自然灾害:对健康有何影响?
厄尔尼诺(ENSO或厄尔尼诺南方涛动)除了导致风暴和洪水的大幅增加,还是诺如病毒引起的感染性腹泻[19]和肠胃炎[20]的重要风险因子。更糟糕的是,厄尔尼诺会造成人口迁移和杂居,从而通过被污染的水体加剧病毒在人群之间、人类和动物之间的传播。霍乱弧菌引起的流行性腹泻得到了重点研究(见图6)。事实上,通过1980年至1998年的一系列观测,研究人员发现孟加拉国霍乱发病率的季节变异与厄尔尼诺现象导致的温度波动相关[21]。
在孟加拉国和秘鲁,霍乱的动态确实与厄尔尼诺波动有关,厄尔尼诺波动似乎与1991年秘鲁再度出现霍乱尤其有关,当时细菌附着在浮游生物上,自西向东横跨太平洋。
2001-2002年的另一件值得关注的事件是马来西亚出现了尼帕病毒,该病毒导致极其严重的出血热,70%的病患死亡。分析认为这一事件是1998年厄尔尼诺肆虐以及该地区森林遭到大量砍伐共同作用的结果[22]。森林遭受破坏后受感染蝙蝠大量逃离导致病毒传播。携带病毒的蝙蝠不会出现症状,但它们很容易传染哺乳动物(如:猪),特别是人类。
汉坦病毒是对气候变化、特别是极端降雨敏感的微生物的另一例证。主要可以引起人类两种疾病:出血热和肾脏综合征(在亚洲和欧洲)和心肺综合征(在北美)(图6)。
2.4. 对水和食物有什么影响?
2.4.1. 导致水源短缺
降水量降低可能会对淡水供应产生影响(参见我们是否面临水资源短缺的风险?)。缺乏安全的饮用水会影响健康,增加患腹泻病的风险,每年有近60万5岁以下儿童死于腹泻。极端情况下,缺水会导致干旱和饥荒。到2090年,受气候变化的影响,干旱地区面积将会扩大,极端干旱情况的发生频率将会翻倍且平均持续时间增加六倍[23]。
洪水发生的频率和强度也在增加,它们污染了淡水资源,增加了水媒疾病的发生风险,并为携带病菌的昆虫的幼虫(如蚊子)创造繁殖场所(见上文)。它们还会造成溺水、身体创伤、房屋损坏以及扰乱医疗保健服务。
2.4.2. 导致食物短缺及营养不良
气温上升、气候事件的影响(生态系统退化、基础设施和人类居住区遭到破坏)……所有这些因素都将对粮食生产造成影响(图7)。世界卫生组织最近的一项研究提到,许多最贫穷地区的粮食产量下降,到2020年,某些非洲国家的粮食产量将下降50%[24]。海平面上升、水源和农业用地的污染(或盐碱化)将加剧这些影响。
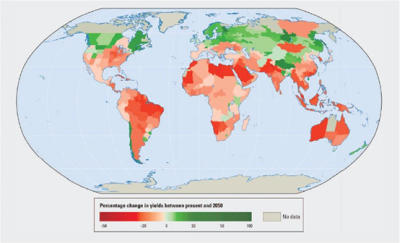
Percentage change in yields between present and 2050.
目前至2050年之间的收益率产量变化百分比。
从较长期来看,气候变化可能会增加作物产量的年际变异性。尽管每年农产品的需求都呈增长态势,但气候变化可能会导致其价格上涨。越来越多的专家关心粮食安全问题。最悲观的预测是,全球作物产量每十年将会减产2%,而2050年前,全球农作物需求量将以每十年增加14%的速度递增。除此之外,取决于气候变暖的程度,影响作物产量的风险预计将进一步增加。总的来说,这将导致营养不良和营养缺乏发生率的增加,目前每年有310万人因上述原因死亡[25]。
2.5. 气候变化对精神健康的影响 -气候难民
2007年诺贝尔和平奖的联合获得者阿尔·戈尔和联合国政府间气候变化专门委员会的专家预测与精神相关的疾病[26](压力,自杀)会增加。气候变化对心理健康的影响已在热浪或异常干旱期间得到证实[27]。据估计,到2050年将有2.5亿气候难民,海平面上升以及住房、医疗设施和其他基本服务遭到破坏导致的人口流动将加剧此类疾病[28]。世界上超过一半的人口生活在距离大海不到60公里的地方!受影响的人口将被迫迁移,这将加剧从精神健康障碍到呼吸及消化系统疾病等各种健康风险。 此外,最近的一项研究提出气温的上升会增加美国的自杀率[29]。这项研究由著名的斯坦福大学的一个研究组展开,分析了1968-2004年美国的自杀率和1990-2010年墨西哥的每月自杀率数据。他们借助气候绘图工具PRISM,将这些数据与美国各县的温度和降水数据进行比较,发现温度上升和自杀风险增加之间存在正相关。
2.6. 永久冻土层融化释放出的微生物?
2016年8月,一名生活在西伯利亚冻原的12岁男孩离开俄罗斯炭疽疫区,后来死于亚马洛-内内西亚自治区首府萨莱克哈德市的一家医院,另有20人也被诊断患有此病。男孩的死因与炭疽病密切关联,炭疽是一种由炭疽杆菌引起的传染病。这名男孩患有肠道型炭疽病,更难诊断,此病在西西伯利亚消失了75年后再次浮出水面。1897年至1925年期间,炭疽杆菌导致驯鹿群大量死亡(150万头驯鹿)并被埋在永冻层中[30],流行病学表明,永冻层融化导致被埋的驯鹿群细菌释放。目前的热浪很可能会导致炭疽孢子(细菌的抗性形式)从填埋区释放。
研究遭受气候变暖影响特别严重的泛北极地区的专家认为其它人畜共患传染病(细菌:布鲁氏菌病、莱姆病、钩端螺旋体病-病毒:狂犬病、汉坦病毒热、蜱传脑炎、西尼罗脑炎)的发病率有可能急剧增加[31]。
2.7. 生物多样性崩溃和对人类健康的影响?
在气候变化及其对人类健康研究中,极少涉及生物多样性的崩溃问题(参见生物多样性不是一种奢侈而是一种必需)。虽然能够确定气候变化对昆虫种群和某些脊椎动物(如鸟类)的影响,但对人类的影响则难以评估。然而,令人震惊的报告指出,生物多样性的衰落将危及全世界人民的经济、生存方式、粮食安全和生活质量[32]。根据其它资料来源,人类自然环境中生物多样性的丧失会让人类健康和生活付出代价,这种代价是隐形的并会毫不留情地传递给后代,可以通过经济学来进行评估[33]。这种代价主要由两个因素引起的:一方面,生物多样性崩溃会导致食用的以及用于保养的生物物质匮乏,另一方面,功能性生态系统遭到破坏甚至崩溃,导致“生态系统”商品和服务的损失。
最后,气候变化对作为生命基础的内源性和环境微生物的影响在很大程度上尚待探究。少量对脊椎动物的研究表明,温度的升高会导致其微生物组的生物多样性减少。同样,海洋酸化会导致了一些无脊椎动物(如海绵多孔动物)的微生物群发生显著变化。一些严肃的假说指出,人类肠道微生物组的改变(参见人类微生物群:我们健康的盟友)和生态失调(与肠道微生物组失衡有关的病理:如炎症性肠病、肥胖、糖尿病等)伴随着全球变化(快速城市化、快餐饮食、远离自然环境的久坐生活方式、大规模抗生素使用、热应激)。
3. 结论:健康、气候变化和全球变化
本章探讨了气候变化对人类健康最明显的影响。有两点需要强调:首先,气候变化对健康影响的测量只能达到非常接近真实的程度,特别是区别于热浪等极端事件的渐变影响(例如对病媒传播疾病的影响),这主要是由于感染源的“不可预测性”。
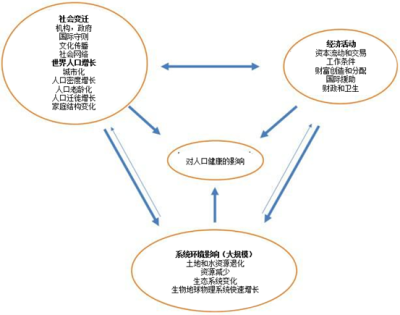
伴随着全球生活方式变化的气候变化本质上已经非常复杂(图8)。这有时使某些预测模型的可靠性存在很大不确性。
另一方面,关于气候变化对健康的影响,我们可以确定以下几点[4]:
- 无论在富裕还是贫穷国家,每年因中暑死亡或住院的人数在增加;
- 病媒传染病或其病媒呈地理扩张态势(如高海拔疟疾);
- 与厄尔尼诺现象有关的沿海地区霍乱流行病的增加;
- 食物格的上涨,特别是在贫困的国家,导致低收入家庭粮食匮乏(贫困陷阱)。
因此,气候变化将对健康产生非常负面的影响,而全球变化的影响将加剧这种影响。所有人都将感受到气候变化的影响,但有些人更容易受到影响,例如:
- 那些生活在小岛屿国家或其它沿海地区、大城市、山区和极地地区的人尤其容易受影响。
- 儿童,特别是生活在贫穷国家的儿童,最容易受到由此产生的健康风险的影响,并将在较长一段时间内受到影响。
对老年人和先前有残疾或疾病的人的健康影响也应更为严重。
表2.与气候变化相关的健康风险总结。
根据世界卫生组织的报告,在没有援助的情况下,缺乏良好卫生基础设施的地区(大多数在发展中国家)将是最没有能力准备和应付这种情况的地区。如果没有重大的改进措施,卫生系统届时将不能应对(例如中暑)。现在唯一负责任的态度是彻底改变我们的经济模式和社会生活方式,对人类和生物多样性(人类健康直接依赖于生物多样性)来说,它已成为一个生死攸关的问题。
参考资料和说明
[1] IPCC. Summary for Policymakers. In: Edenhofer O, R. Pichs-Madruga, Y. Sokona, E. Farahani, S. Kadner, K. Seyboth, A. Adler, I. Baum, S. Brunner, P. Eickemeier, B., Kriemann JS, S. Schlömer, C. von Stechow, T. Zwickel and J.C. Minx editors (2014), Climate Change 2014, Mitigation of Climate Change Contribution of Working Group III to the Fifth Assessment Report (AR5) of the Intergovernmental Panel on Climate Change. Cambridge, United Kingdom and New York, NY, USA, Cambridge University Press
[2] Smith KR et al (2014) Human Health: Impacts, adaptation, and co-benefits. In Climate change: Impacts, Adaptation, and vulnerability. Part A: Global and Sectoral aspects. Contribution of Working Group II to the 5th assessment Report (AR5) of the Intergovernmental Panel on Climate change. Field CB et al (eds), Cambridge University Press, UK pp 709-754
[3] Costello A et al (2009) Managing the health effects of climate change. Lancet 373: 1693-1733
[4] McMichael AJ (2013) Globalization, climate change and Human Health. New Engl J Med 368: 1335-1343
[5] Schär C (2004) The role of increasing temperature variability in European Summer heatwaves. Nature 427: 332-336
[6] Robine JM et al (2008) Death toll exceeded 70,000 in Europe during the summer of 2003. Reports/Biology Series, 331:171-78
[7] Wimberly et al (2014) Regional variation of climatic influences on West Nile virus Outbreaks in US. Am. J Too much. Med Hyg. 91: 677-684
[8] Mora C et al (2017) Global risk of deadly heat. Nature Climate Change. doi:10.1038/nclimate3322
[9] Zhang Y, Hansen A, Bi P. (2014) Climate change and vector-borne viral diseases. In Viral infections and global change. Singh SK ed John Wiley & sounds Hoboken, New Jersey
[10] Kraemer MU et al (2015) The global distribution of the arbovirus vectors Aedes aegypti and Ae. albopictus. Elife 4:e08347
[11] Hales S et al (2002) Potential effect of population and climate changes on global distribution of dengue fever: an empirical model. Lancet 360:830-4
[12] Schaffner F & Mathis A (2014). Dengue and dengue vectors in the WHO European region: past, present, and scenarios for te future. Lancet Infect Dis 14: 1271-1280
[13] Bhatt S et al (2013) The global distribution and burden of Dengue. Nature 496: 504-507
[14] Harrigan RJ et al (2014) A continental risk assessment of West Nile Virus under climate change. Global Change Biology 20: 2417-2425
[15] Weaver S (2013) Urbanization and geographic expansion of zoonotic arboviral diseases: mechanisms and potential strategies for prevention. Trends Microbiol. 21(8):360-3.
[16] Paz S. & Semenza J.C. (2016) El Niño and climate change-contributing factors in the dispersal of Zika virus in the Americas? Lancet 387(10020):745
[17] Jonathan A. Patz & William K. Reisen (2001) Immunology, climate change and vector-borne diseases. Trends in Immunology Vol.22 No.4 April 2001
[18] Lindsay S.W. & Martens W.J. (1998) Malaria in the African highlands: past, present and future. Bull World Health Organ. 76(1):33-45
[19] Pascual M. et al (2000) Model relationship between ENSO and cholera in Bangladesh (Int. Center For Diarrhoeal disease Research, Bangladesh) Science, 289(5485):1766-9.
[20] Chrétien J.P. et al (2015) Global climate anomalies and potential infectious disease risks. Plos Current outbreaks doi: 0.1371/currents.outbreaks.95fbc4a8fb4695e049baabfc2fc8289f
[21] Rodo X et al (2002) ENSO and cholera: a non stationary link related to climate change? Proc Natl Acad Sci USA 99(20):12901-6.
[22] Chua KB et al (2002) Anthropogenic deforestation, El Niño and the emergence of Nipah virus in Malaysia. Malays J Pathol. 24(1):15-21.
[23] Food Policy Report No. 21, September 2009. International Food Policy Research Institute (IFPRI) IPCC Fourth Assessment Report: Climate Change 2007 (AR4)
[24] WHO (2014) Quantitative risk assessment of the effects of climate change on selected causes of death, 2030s and 2050s. Geneva: World Health Organization
[25] Wheeler T & von Braun J. (2013) Climate change impacts on global food security. Science 2013;341:508-13
[26] Levy BS & Patz JA (2015) Climate change, Human rights and social justice. Annals Global Health 81, 3: 310-322
[27] Berry H.L., Bowen, K & Hjellstrom T. (2010) Climate change and mental health: a causal pathways framework. Int J Public Health. 55(2):123-32.
[28] Black R, Bennett SR, Thomas SM, Beddington JR (2011) Climate change: Migration as adaptation. Nature 478:447-9.
[29] Burke M et al (2018). Higher temperatures increase suicide rates in the United States and Mexico. Nature Climate change 8: 723-729
[30] Revich BA & Podolnaya MA (2011) Thawing of permafrost may disturb historic cattle burial grounds in east Siberia. Global Health Action doi: 10.3402/gha.v4i0.8482. Epub 2011 Nov 21
[31] Parkinson AJ, Evengard B, Semenza JC, et al (2014) Climate change and infectious diseases in the Arctic: establishment of a circumpolar working group. Int J Circumpolar Health. doi: 10.3402/ijch.v73.25163.) e(31
[32] https://www.who.int/globalchange/ecosystems/biodiversity/fr/
[33] http://sante-biodiversite.vetagro-sup.fr/wp-content/uploads/HB-REVUE2015HS_web-aout-20153.pdf
环境百科全书由环境和能源百科全书协会出版 (www.a3e.fr),该协会与格勒诺布尔阿尔卑斯大学和格勒诺布尔INP有合同关系,并由法国科学院赞助。
引用这篇文章: DROUET Emmanuel (2024年3月9日), 气候变化:对我们的健康有什么影响?, 环境百科全书,咨询于 2025年2月2日 [在线ISSN 2555-0950]网址: https://www.encyclopedie-environnement.org/zh/sante-zh/climate-change-what-effects-on-health/.
环境百科全书中的文章是根据知识共享BY-NC-SA许可条款提供的,该许可授权复制的条件是:引用来源,不作商业使用,共享相同的初始条件,并且在每次重复使用或分发时复制知识共享BY-NC-SA许可声明。